|
Research Article
Perioperative care in COVID-19 patients requiring emergency surgical procedures: A systematic review
1 Final Year Student, College of Medicine, University of Ibadan, Ibadan, Oyo State, Nigeria
2 Consultant Orthopaedic Surgeon, Department of Orthopaedic Surgery, University College Hospital, Ibadan, Oyo State, Nigeria
Address correspondence to:
Olubunmi Emmanuel Odeyemi
College of Medicine, University of Ibadan, Ibadan, Oyo State,
Nigeria
Message to Corresponding Author
Article ID: 100044S05OO2020
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Odeyemi OE, Eyitayo JO, Oyesiji EM, Balogun M. Perioperative care in COVID-19 patients requiring emergency surgical procedures: A systematic review. Edorium J Surg 2020;7:100044S05OO2020.ABSTRACT
Aims: The novel coronavirus infection (COVID-19) was first discovered in Wuhan, Hubei province, China and has spread to various continents of the world. This pandemic has beyond doubt affected patient care as reallocation of resources to the care of COVID-19 patients is now the order of the day.
Methods: We conducted a systematic review to identify demands of conducting surgical procedures during the COVID-19 pandemic. Our search strategy involved using the following databases: PubMed, MEDLINE, Google Scholar, and other medical databases. The search terms were “COVID-19,” “surgery,” “COVID-19 and Surgery.” Titles and abstracts of articles available in English were examined. The identified full texts were screened for original data, and related references were retrieved and checked for relevancy based on the inclusion criteria.
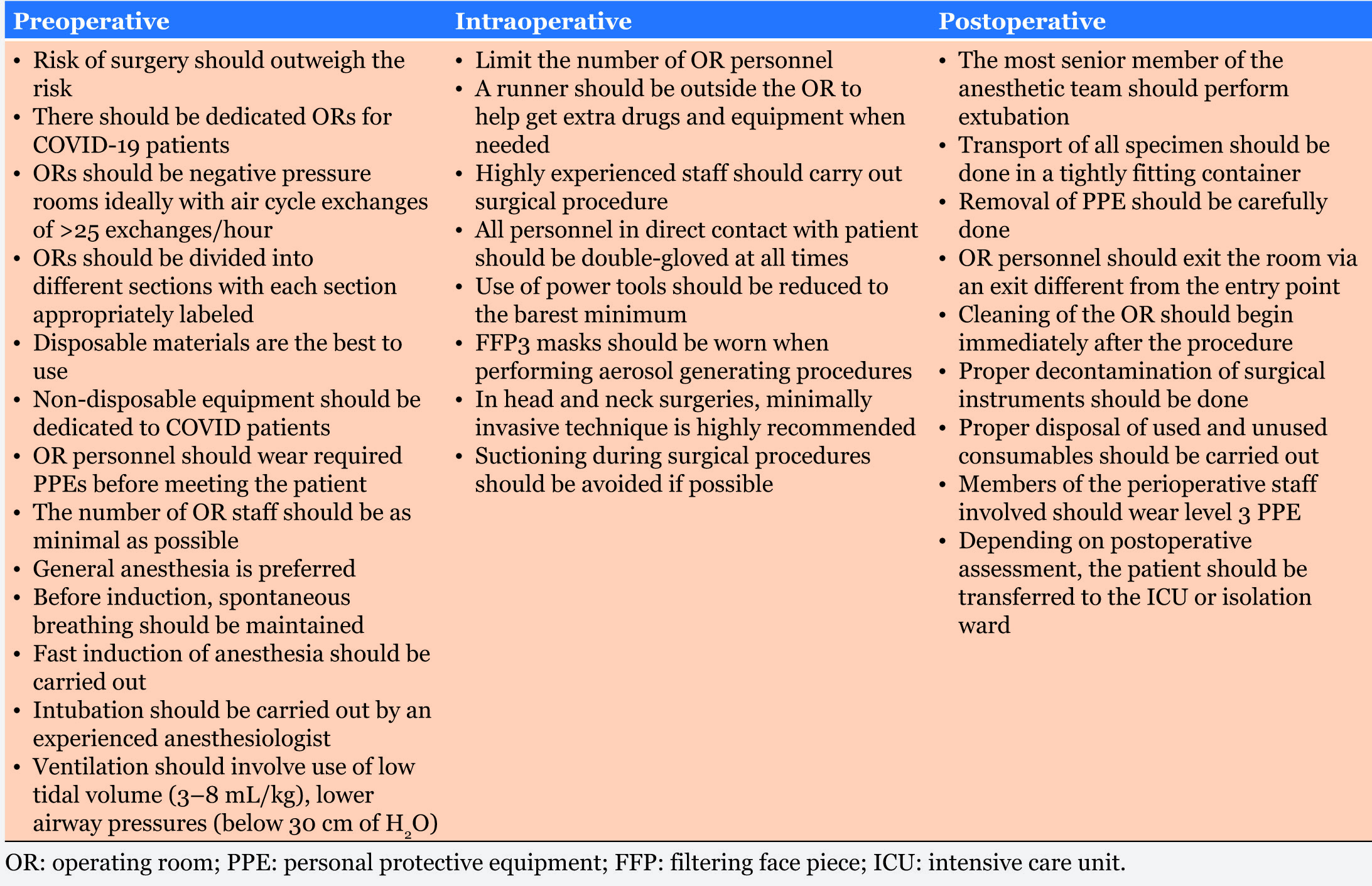
Results: Studies that met the inclusion criteria were thoroughly reviewed. We gathered that COVID-19 has greatly impacted the perioperative management of patients requiring emergency procedure during the pandemic. Preoperatively, venues and materials needed for surgery, including surgical personnel have been defined. There is also significant impact on intraoperative activities including ventilation of the patient, use of some equipment that could cause aerosol generation, and also postoperative care of the COVID-19 patient.
Conclusion: This study provides a framework for navigating through the muddy waters of performing surgery on COVID-19 infected patients, with emphasis placed on the prevention of cross-transmission in the hospital. All hands therefore must be on deck at every stage of management of COVID-19 infected patients.
Keywords: Anesthesia, COVID-19, Health care workers, Surgery, Transmission
INTRODUCTION
The novel coronavirus outbreak began in Wuhan, China in December 2019. As a result of its rapid spread to other parts of the world, the World Health Organization (WHO) declared the virus as a pandemic on March 11, 2020. Currently, there has been over 5 million reported cases and more than 300 thousand confirmed deaths as a result of this deadly virus worldwide [1]. Now popularly called COVID-19 [2], the virus has caused a global disarray, shaking nations and having not only health impact but also economic and political implication [1],[3],[4].
The overall case fatality rate of COVID-19 is about 1.4%, however, the risk of death in individual infected increases with increasing age with about case fatality ratio (CFR) of 1% in children less than 10 years of age to 8% in those who are 80 years old and above [3].
COVID-19 is a viral respiratory infection whose clinical features are closely related to the influenza H1N1 [5],[6] and it runs a clinical cause similar to those of Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS), which were also declared pandemic between 2000 and 2003 [7],[8],[9]. While its mode of transmission is not fully understood, transmission from contact with infected persons has been documented [7],[8],[9].
Also known as SARS-CoV2, the documented risk factors for COVID-19 are extremes of ages, chronic diseases such as diabetes mellitus (DM) [10], coronary artery disease (CAD), cerebrovascular disease (CVD), chronic obstructive pulmonary disease (COPD), and cancers. Males are also at higher risk than females [11], with extremes of ages and presence of other comorbidities being highly correlated with increased CFR [7],[12],[13],[14],[15],[16].
Infected individuals can manifest the signs and symptoms ranging from fever, dry cough, headache, and respiratory distress [9],[15]. Other documented clinical features include sore throat, fatigue, lethargy, diarrhea, and chest tightness [15], while some other infected persons may remain asymptomatic throughout the incubation period with the ability to transmit the infection to others [17], with incubation period of COVID-19 being between 2 and 14 days [8],[18],[19]. Given that the symptomatology is closely related to other viral respiratory infections such as flu, MERS, SARS, this poses a challenge on early detection and diagnosis of COVID-19 [14],[20],[21]. The most pronounced feature of SARS-CoV2 is acute respiratory distress syndrome (ARDS) [8],[14],[20],[22],[23], increasing the need for mechanical ventilation in those infected. The impact of COVID-19 outbreak on patient requiring any form of medical care is pronounced, with the attention of health care team being shifted to combating COVID-19 outbreak [24]. It has been recommended that all elective surgeries be cancelled [15],[25],[26],[27],[28],[29]. About 10% of SARS-CoV2 infected patients will require intensive care unit (ICU) admission, of which 20% will require one form of surgical procedures or the other [30],[31]. Of the percentage that had operative procedures done, only about 30% will eventually survive [30],[32], with most patient dying from complications arising from these procedure [31]. Any form of surgical procedure is a stressor to the patient. Therefore, patients with COVID-19 needing operative procedures are not only at higher risk of transmitting the infection to others (health care team) [30], they may also experience exacerbation of symptoms, and are sometimes more prone to death resulting from the infection following these procedures [13],[28]. Despite the documented evidences concerning COVID-19 infected patient requiring any form of operative procedure during their period of care, there is however paucity of data concerning precautionary measures needed to be taken during such procedure. In order to minimize infection transmission and to improve outcome [30],[32], the managing team must be informed of what needs to be put in place, necessitating this review [33].
Several articles have addressed different parts of the demand of operative procedure. Based on the existing body of knowledge, this review will be putting to the perspective of the peri-, pre-, intra-, and postoperative demands and measures required to minimize transmission of infection to the medical team and to improve patient outcome.
MATERIALS AND METHODS
Literature search strategy
A systematic electronic literature search was carried out by two independent individuals first on April 6 and was repeated for the last time on May 26, 2020. PubMed, MEDLINE, Google Scholar, and other related medical databases were searched using the following search terms: “COVID-19,” “Surgery and COVID-19,” “Coronavirus,” “SAR-CoV2,” “SARS-CoV2 and Surgery,” and “Surgical procedure in COVID-19.” The search was limited to manuscripts published in English language. We examined titles and abstracts of articles that were available in English language.
Inclusion and exclusion criteria
Two reviewers evaluated the topic and the abstract of the articles and the relevance of the articles were determined. Articles initially recruited for the review were selected based on meeting any of the inclusion criteria: Published online on COVID-19 between December 2019 and May 26, 2020, addressing component of the perioperative management of COVID-19 patient, and focusing on either minor or major surgical procedures relating to management of COVID-19 patient. However, final article selection was done based on meeting the first criterion and either second or third criterion. The retrieved results were jointly cross-examined and disagreements were solved by discussions among the team members. Articles that did not meet the inclusion criteria such as those addressing the epidemiology and clinical characteristics were excluded from the review.
Data extraction
Having gone through various screening stages, we selected articles that met the inclusion criteria as stated above. Three reviewers independently examined the literatures with each focusing on the preoperative, intraoperative, and the postoperative aspect of the articles and the data was subsequently extracted and collated.
RESULTS
1. Preoperative
Risk assessment
It has been shown that surgical procedures can increase the rate of disease progression especially in previously asymptomatic patients and also that the mortality rate is higher in this category of patients [30],[34]. Therefore, the need for the surgical procedure must be objectively assessed, ensuring that the benefit of the procedure outweighs the associated risk. Elective surgical procedures should be postponed as this would help preserve scarce resources including personal protective equipment (PPE) and also maintain treatment space for critical patients [34],[35],[36],[37]. Also recommended is that all elective procedures that may result in aerosolization be deferred and if indicated, appropriate PPEs should be worn [13],[38],[39],[40],[41]. COVID-19 pandemic is associated with fear, therefore, aversion for surgery may increase in them. As a result, pragmatic steps must be taken to ensure that patient is calm and less anxious prior to the procedure [42].
Operating room
It is important that each hospital has dedicated operating areas to COVID-19 patients requiring urgent/emergent surgeries. Operating rooms closest to the entrance of the theatre block should be the designated ones to this category of patients [15],[43],[44]. Minimally invasive procedures for COVID-19 patients should be done in separate rooms different from the uninfected patients [38],[40],[45].
However, it is recommended that if a hospital has provisions for satellite operating complexes, they should be deployed for the use of COVID-19 patients as this would reduce the risk of contamination of other operating rooms (ORs) [46]. While in transit, the COVID-19 positive patient should move directly to the dedicated OR without stopping at any other place [15],[24],[44]. Negative-pressure OR (below 5 Pa) is required as this would be ideal to prevent dissemination of the virus [32],[35],[43],[46],[47]. More so, high-efficiency particulate air (HEPA) filters can be placed in positive pressure operating rooms. In addition to this, a high air exchange cycle rate (≥25 cycles/hour) will effectively reduce the viral load in the operating room [6],[38],[44],[46]. This is especially important for aerosol generating procedures. Also, in positive-pressure ORs, the clean air conditioning system should be shut off [35],[38].
The OR complex should be divided into different sections: the entry dressing room, where the basic PPE is worn, the anteroom, where disinfection and surgical dressing take place, the operating room itself, the exit room where PPE is removed, and the exit dressing room where the staff can shower. Each room should be properly labeled to enhance distinctness [46].
The selection of equipment
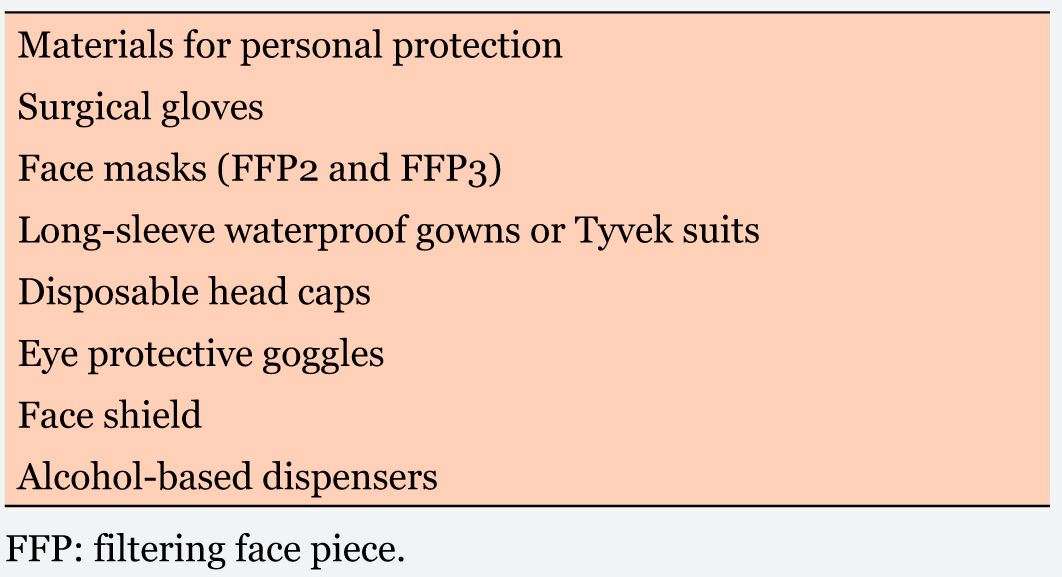
Disposable supplies are the best choice to use for this category of patients [35],[44]. Disposables needed for surgical procedures include gloves, face masks (FFP2 and FFP3), eye protective goggles, disposable long-sleeved waterproof gowns or Tyvek suits, face shield, disposable head caps, and alcohol-based dispensers (Table 1). When gloves have been contaminated, they should be discarded and replaced so as not to contaminate other surfaces [13],[15],[26],[31],[38],[43],[44],[48].
Concerning the non-disposable equipment, it is recommended that their use be dedicated to COVID-19 patients only, that is, they should remain in the OR reserved for COVID-19 patients. These include the anesthetic machines, nebulizers, humidifiers, and so on [35],[43],[48]. It is advised that heat and moisture exchangers be placed on the expiratory limb of the breathing circuit, and both the heat and moisture exchanger filters and the soda lime should be changed after each procedure [38],[43].
OR personnel
All OR staff have to wear the required PPEs before meeting the infected patient. It is very important to take precautions during the intraoperative period to protect the patient and the operating room staffs. Whether a case is being suspected or it has been confirmed already, they must be treated as positive until proven otherwise in order to minimize spread of infection. Dedicated senior staff should be allocated to important management roles and all staff should have proper training on the use of PPEs [6],[31],[40]. This consideration must be made across all surgical modalities. Also, it is very important that the number of people working in a particular dedicated operating room should be as minimal as possible [35],[44].
It is important that once the patient is in the operating room, the door should be shut. It is also very important that all the personnel involved in the surgery enter in a timely manner, that is, entering the suite when their services are needed as this would minimize the time spent with the patient [6],[38]. Also, it is imperative to avoid moving out of the operating suite until the end of the procedure. Each health care worker must be properly dressed in their PPEs before coming in contact with the patient [6],[38],[44],[45]. In addition to wearing of protective materials, they should take universal precautions [48]. During the procedure, a runner nurse should be stationed outside the operating room just in case additional drugs or equipment will be needed. These will be placed on a trolley that will be left in the anteroom for the OR team to retrieve [43].
The choice of anesthesia procedures and the management
In COVID-19 patients, general anesthesia or monitoring anesthesia is usually adopted. The principle is that adequate oxygen supply should be maintained, anesthetic agents should be adequate, cough reflex and agitation should be avoided and the safety of the patient and staff should be ensured. While preparing to induce the patient, spontaneous breathing and oxygen inhalation by continuous positive airway pressure (CPAP) should be maintained [35],[38].
It is recommended that fast induction of anesthesia should be performed to prevent the patient from coughing. Induction agents should be administered in this order: muscle relaxants, intravenous general anesthetic agents, and opioids to avoid cough [32]. Patients who are yet to be intubated should put on a face mask until induction [15],[44]. Intubation should be carried out by an experienced anesthesiologist and awake intubation techniques should be avoided. This will help to avoid failed attempts and improve first-time success rate. Of note is that unless it is specifically indicated, fiber-optic intubation should be avoided [44]. There could be occasions of difficult airways in which case a laryngeal mask should be placed after the first failed attempt. After an anesthetist has intubated the patient, end-tidal CO2 and chest rise are the best indicators of correct intubation. For the ventilator settings after intubation, it is recommended to use lower tidal volumes (3–8 mL/kg), lower airway pressures (below 30 cm H2O), and higher frequency ventilation to protect the lungs. If manual ventilation is needed small current volumes should be used [35],[44],[48].
In pediatric patients, because they may be anxious when separated from parents which could result in crying and spraying of saliva, midazolam or dexmedetomidine should be administered before the patient enters the operating room. Also, intravenous sedatives or masked inhaled sevoflurane should be used for induction [35].
For American Society of Anesthesiologists (ASA) class I–II patients, intravenous anesthesia combined with regional nerve block or caudal without intubation is recommended excluding brain surgery, craniofacial, cardiothoracic, ear-nose-throat, and laparoscopic surgeries. Patients in ASA class III or above should be anesthetized with tracheal intubation with general anesthesia [35],[42].
2. Intraoperative
Personnel
Limit the number of personnel in the OR to essential staff only [24],[31]. The OR doors must be closed as soon as the patient enters and individuals should remain in the OR until the surgery is over [24],[44].
A runner nurse should be stationed outside the OR to help get extra drugs and equipment when needed. There is an anteroom with a trolley where this individual places the needed items while wearing PPE. This trolley can also be used to send out specimens like arterial blood gases sample [43].
Highly experienced staff with pre-established routines are preferred in carrying surgical procedures like tracheostomy [15],[47]. This coupled with efficient communication between team members would quicken operating time and thus minimize the chance of transmitting the virus by reducing exposure time [6],[39].
The surgeon and other members of the team should only be allowed to enter the OR after adequate disinfection and dressing [46]. All personnel in direct contact with the patient must wear a double pair of latex gloves at all times [44].
Procedure
The surgical treatment of trauma and Orthopaedic cases involves the use of power tools like drills, bone saws, reamers, and electrocautery. The use of these tools should be minimized because they generate aerosols which can facilitate virus spread. It is advised that these tools are operated at low power settings [31],[46],[49].
Special precautions should be taken when involved in procedures associated with increased risk of transmission. An FFP3 mask should be worn before procedures like endotracheal intubation, noninvasive ventilation, tracheostomy, cardiopulmonary resuscitation, manual ventilation before intubation, and bronchoscopy [24],[34],[41],[45]. These procedures are high risk because they are very likely to release aerosols [38],[41],[44]. During tracheostomy, it is advised that exposure time to aerosolized secretions be reduced by ensuring complete paralysis of the patient throughout the procedure, stopping mechanical ventilation just before entering the trachea and minimizing suction use during the procedure [13],[45],[47]. Open tracheostomy is preferred to percutaneous tracheostomy due to the lesser chance of aerosolization [41],[47]. Thomas-Rüddel et al also advocate for sufficient relaxation of the patient before tracheostomy [15]. Smoke extraction devices should be used with caution because they have the potential to increasing aerosol generated during intraoperation [24],[31],[40],[49]. Where and when available, a triple filter system should be used [39].
In the treatment of head and neck tumors, minimally invasive approach is highly recommended [31],[42]. This helps to reduce duration of surgery. Surgical defects should also be reconstructed with local flaps rather than revascularized flaps [50]. Incision and port sites should be managed well to avoid escape of air from the peritoneum during laparoscopic procedures. Also, number of skin incisions must be minimized and of moderate sizes to fit the endoscopic devices. Insufflations must be done with care. Insertion and removal of the troca should be carefully done to avoid spillage of body fluids [24],[39]. Aerosolization of the coronavirus increases during endoscopic sinus surgery and skull base surgery, hence, all endoscopic procedures should be postponed unless considered necessary [38]. If these procedures must be carried out, oral and nasal mucosa must be adequately anesthetized using anesthetic pledgets instead of anesthetic sprays in order to reduce cough and sneeze reflex. Also, it is preferable to use smallest diameter scopes for these procedures so as to reduce coughing and sneezing. Appropriate PPE for aerosol exposure is recommended [13],[38].
Suctioning during surgical procedures should be avoided if possible [47]. If suction is to be used, suction devices with the ability to remove smoke and aerosols should be made available during aerosol generating procedures [46]. Suction used within a closed system is recommended [15],[24],[40],[47],[51], preferably with a viral filter [47].
3. Postoperative
This period is marked by the end of the surgical procedure and the initiation of anesthesia reversal. Removal of the PPE by any member of the operating team must be carefully done in a stepwise manner [43],[44],[46]. After removal of a layer of the PPE, the hand must be disinfected with alcohol-based sanitizer before the removal of the next layer [46]. This phase is very important because the risk of transmitting the infection is very high, therefore, all precautions need to be strictly adhered to. It is recommended that medical team should exit the operating room via an exit that is different from the entry point [46].
The most senior member of the anesthetic team commences the extubation of the patient, while doing this, full level 3 PPE with N95 or PAPR must be worn because there is a risk of coughing from the irritation of the airway thereby increasing the risk of infection transmission. Transport of all specimen must be done in a tightly fitted container [13],[15],[42],[44],[46],[52].
Waste disposal and cleaning of the operating room
Cleaning of the operating room must begin immediately the procedure is over. This begins with the decontamination of the anesthetic equipment [30],[32],[48]. Operating table, tray surfaces, and other reusable materials must be well decontaminated with alcohol-based sanitizer [44],[46]. Surgical instruments must be washed, dried, decontaminated, packed in a sealed container and sent for sterilization immediately after the procedure [46].
After the surgical procedure is over, proper cleaning and disposal of used and unused consumables that may be regarded as contaminated must begin. While still adequately protected by PPE, all consumables to be disposed must be packed and sealed in a container [42],[44]. Any unused drugs or other consumables present in the OR must be assumed contaminated and therefore disposed [30],[32],[44],[46],[47]. It is recommended that such container is labeled for easy recognition and for possible awareness to others [42],[44],[46]. Having carefully packed the waste into a labeled and sealed container, it is then transported by an assigned perioperative staff to a designated COVID-19 point of disposal [6],[13],[35],[42],[44]. During the transportation of the waste, all precautionary measures must be ensured and contact with other surfaces must be avoided to reduce the risk of transmission of the disease [42],[44]. The waste disposal area for COVID-19 related waste must be separate and easily identifiable. Members of the perioperative staff saddled with these responsibilities must wear their level 3 PPEs [6],[13],[43],[44],[46],[50].
Planning for a next procedure can be exceptionally stressful with full repeat of all the precautionary measures. Usually, an interval of 1–3 hours is recommended before the start of another procedure using the same operating room [44]. This recommendation is based on the pervasiveness of aerosol of COVID-19 in air. It can stay much longer on surfaces. Adequate interval also gives room for reusable materials to be well sterilized [42].
Patient transfer and monitoring
After each procedure, the transportation of patient is done and the decision of whether patient is taken to ICU or isolation ward is based on the preoperative and immediate postoperative assessment by the managing team [30],[42],[43]. During the process of transiting from the OR, patients must have their PPEs on especially with N95 mask, and contact with other animate or inanimate object must be minimized [42]. Passages must be disinfected immediately. Patient who had aerosol generating procedures must be isolated. While in the Isolation ward or ICU [42],[44],[48],[50], each visit to patient must be kept short and targeted at meeting specific needs of the patient [37],[44],[46]. Hand washing facilities should be present at the entrance to the ward and also at patient’s bedside [6]. Number of visiting medical team for a visit must be reduced and visiting members must have their PPEs worn and have their hands sanitized before and immediately after attending to the patient [42],[46]. Wearing of double gloves is recommended for perioperative staff who will be handling patient’s blood, urine, and other secretions [44],[46],[50].
DISCUSSION
In the face of the ongoing pandemic, the safety of the medical team is of utmost priority while improving outcome of those infected with the disease [26],[53]. With health practitioners being at the forefront in the fight against COVID-19 pandemic, there is a need for not only for an institutionalized or local protocol but a well-defined, basic guidelines that govern the interactions of physicians with their patients [6],[38]. Since the onset of COVID-19 pandemic, there has been an increase in the number of health care workers dying from being infected with the disease. Since the onset of COVID-19 pandemic, there has been increase in the number of health care workers dying from the disease [7],[12],[42],[54] (Table 2).
The goal of inpatient care of COVID-19 patient is to improve their outcome, minimizing infection transmission to the healthcare team. Based on the documented knowledge, this review further highlights the implication and the rudiments of all that needs to be put in place in managing COVID-19 patient needing any form of surgical procedure [27],[41],[47],[55]. It also provides a framework for navigating through the muddy waters of performing surgery on COVID-19 infected patients, with emphasis placed on the prevention of cross-transmission in the hospital [35],[42],[44],[46]. An important first step in the prevention of COVID-19 among surgical patients and their care providers is the postponement of all elective procedures [27],[29],[42],[43],[44],[46]. Risk stratification is of essence [27],[47], comparing the benefit of the procedure with the associated risk. Irrespective of the indication for the procedures, all patients must be treated as positive for the disease, hence, the need for adequate precautionary measures on the part of the attending health care workers [7],[22],[36],[46]. So all emergency surgical procedures must be approached as a case of COVID-19 [37],[44]. Adequate first responder system must be in place to attend to new admission. While performing their duties, clinicians must understand how predisposed they are without adequate self-protection.
It is not enough to have a dedicated room for operative procedures, an interval of 1–3 hours or more should be between cases due to the pervasiveness of COVID-19 aerosols in the air and much more on surfaces [8],[13],[23],[32],[42],[46]. However, other OR that meets the requirement needed can be used in the face of urgency. First, the choice of surgical modality must be determined. Open procedures have been recommended above endoscopic ones largely due to the more aerosol-generating nature of latter [24],[49] which may increase the risk of cross-infections between patient and OR personnel [6],[24].
There are no enough evidences to substantiate the presence of COVID-19 RNA in smokes generated during electrosurgery and other endoscopic procedures. However, there are also no enough data to the contrary [41]. Therefore, minimally invasive surgical modalities should be considered only when the benefits outweigh the associated risk to the patient and health care personnel [24],[38],[49],[51],[56]. Though more aerosols generating, minimally invasive procedures may help to reduce the number of OR personnel with minimal tissue damage and body fluid loss thereby reducing risk of cross-infection intraoperatively and shortening patient recovery time which may be of advantage in centers with limited facilities for patient admission [31],[39],[51]. Prioritizing patients care while maintaining infection control will help arrive at a better choice.
Stricter measures need to be taken when performing aerosol generating procedure and other procedures involving the head and neck region [29],[44],[47].
There is paucity of data concerning COVID-19 patients needing organ transplant during their care. When organ transplant is required as a life-saving process, both the recipient and the donor must be tested and cleared of COVID-19 [57],[58],[59]. It is recommended that transplantation surgeries should not hold but be deferred in a patient with COVID-19 [59],[60]. This submission is due to the potential negative impact of these procedures on the outcomes of this group of patients [60]. However, it is recommended that transplantation surgery should not hold and should be deferred in a patient with COVID-19 [59],[60].
LIMITATIONS OF THE STUDY
As at the time of this review, and the period of literature search, only few literatures have been published on the subject of interest. This poses a limitation to this study. However, with rapid increase in the advancement in knowledge of the COVID-19 and the quest to understand better precautionary measures and management approaches of infected individuals daily, more insight will be gained, hence, the recommendations. Also, there may be unpublished works which are unavailable to us. A limitation of this study is the inability to address the management of non-COVID-19 surgical patients who need non-emergent life-saving treatment, for example, patients with chemosensitve tumors who need chemotherapy or patients with resectable malignancies. The implications of this neglect cannot be completely elucidated until the pandemic is over. Furthermore, the article does not address the anesthetic complications peculiar to COVID-19 patients that may arise postoperatively and how to manage them. In addition, the article does not address the peculiarities of managing COVID-19 in resource poor centers. Many of the materials and infrastructure needed to prevent the spread of the virus in developing countries are mostly unavailable.
RECOMMENDATIONS
Given the peculiarities of various medical facilities globally, and the differences in the resources available, we recommend that these protocols are modified to suit the various practicing conditions that may be in immediate reach of the physicians. Hence, the findings in this review present a guide to the elementary requirement for enhancing health workers’ safety as they give their all to managing COVID-19 patients. We also advise that protocols and treatment guidelines are validated by heads of departments or any other local bodies capable of assuming such responsibility. Review of the treatment guidelines in various settings is done from time to time in order to ensure effectiveness and functionality. Therefore, treatment guidelines should be flexible enough to accommodate for adjustment when necessary. This is also a wakeup call to policy makers in resource poor nations to rise up to the challenge and provide necessary equipment to health care workers who would help mitigate the spread of the virus.
CONCLUSION
Emergency surgical procedure on a COVID-19 patient may be necessary in the course of care. Surgeons and other health care workers will give their best to COVID-19 patient care if their safety is guaranteed. Therefore, necessary and adequate protective measures must be put in place to ensure safety of perioperative team members.
REFERENCES
1.
Coronavirus disease (COVID-19): Situation report – 126. [Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200525-covid-19-sitrep-126.pdf?sfvrsn=887dbd66_2]

2.
Coronavirus disease 2019 (COVID-19): Situation report – 51. [Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10]

3.
Ciotti M, Angeletti S, Minieri M, et al. COVID-19 outbreak: An overview. Chemotherapy 2020;1–9. [CrossRef]
[Pubmed]

4.
Açikgöz Ö, Günay A. The early impact of the Covid-19 pandemic on the global and Turkish economy. Turk J Med Sci 2020;50(SI-1):520–6. [CrossRef]
[Pubmed]

5.
Kong WH, Li Y, Peng MW, et al. SARS-CoV-2 detection in patients with influenza-like illness. Nat Microbiol 2020;5(5):675–8. [CrossRef]
[Pubmed]

6.
De Simone B, Chouillard E, Di Saverio S, et al. Emergency surgery during the COVID-19 pandemic: What you need to know for practice. Ann R Coll Surg Engl 2020;102(5):323–32. [CrossRef]
[Pubmed]

7.
Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA 2020. [CrossRef]
[Pubmed]

8.
Battegay M, Kuehl R, Tschudin-Sutter S, Hirsch HH, Widmer AF, Neher RA. 2019-novel coronavirus (2019-nCoV): Estimating the case fatality rate – a word of caution. Swiss Med Wkly 2020;150:w20203. [CrossRef]
[Pubmed]

9.
Zhao D, Yao F, Wang L, et al. A comparative study on the clinical features of COVID-19 pneumonia to other pneumonias. Clin Infect Dis 2020;ciaa247. [CrossRef]
[Pubmed]

10.
Spinelli A, Pellino G. COVID-19 pandemic: Perspectives on an unfolding crisis. Br J Surg 2020;107(7):785–7. [CrossRef]
[Pubmed]

11.
Sun P, Lu X, Xu C, Sun W, Pan B. Understanding of COVIDâ€19 based on current evidence. J Med Virol 2020;92(6):548–51. [CrossRef]
[Pubmed]

12.
Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020;395(10229):1054–62. [CrossRef]
[Pubmed]

13.
Vukkadala N, Qian ZJ, Holsinger FC, Patel ZM, Rosenthal E. COVID-19 and the otolaryngologist: Preliminary evidence-based review. Laryngoscope 2020;1–7. [CrossRef]
[Pubmed]

14.
Pal R, Bhadada SK. COVID-19 and non-communicable diseases. Postgrad Med J 2020;1–2. [CrossRef]
[Pubmed]

15.
Thomas-Rüddel D, Winning J, Dickmann P, et al. Coronavirus disease 2019 (COVID-19): Update for anesthesiologists and intensivists march 2020. Anaesthesist 2020;1–10. [CrossRef]
[Pubmed]

16.
Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med 2020;46(5):846–8. [CrossRef]
[Pubmed]

17.
Guo X, Wang J, Hu D, et al. Survey of COVID-19 disease among orthopaedic surgeons in Wuhan, People’s Republic of China. J Bone Joint Surg Am 2020;102(10):847–54. [CrossRef]
[Pubmed]

18.
Young BE, Ong SWX, Kalimuddin S, et al. Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. JAMA 2020;323(15):1488–94. [CrossRef]
[Pubmed]

19.
Leung NHL, Chu DKW, Shiu EYC, et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med 2020;26(5):676–80. [CrossRef]
[Pubmed]

20.
Murthy S, Gomersall CD, Fowler RA. Care for critically ill patients with COVID-19. JAMA 2020;323(15):1499–1500. [CrossRef]
[Pubmed]

21.
Morris SN, Fader AN, Milad MP, Dionisi HJ. Understanding the [CrossRef]
[Pubmed]

22.
Verity R, Okell LC, Dorigatti I, et al. Estimates of the severity of coronavirus disease 2019: A model-based analysis. Lancet Infect Dis 2020;20(6):669–77. [CrossRef]
[Pubmed]

23.
Wu JT, Leung K, Bushman M, et al. Estimating clinical severity of COVID-19 from the transmission dynamics in Wuhan, China. Nat Med 2020;26(4):506–10. [CrossRef]
[Pubmed]

24.
Mallick R, Odejinmi F, Clark TJ. Covid 19 pandemic and gynaecological laparoscopic surgery: knowns and unknowns. Fact Views Vis Obgyn 2020;12(1):3–7.
[Pubmed]

25.
Pellino G, Spinelli A. How coronavirus disease 2019 outbreak is impacting colorectal cancer patients in Italy: A long shadow beyond infection. Dis Colon Rectum 2020;63(6):720–2. [CrossRef]
[Pubmed]

26.
Cohen SL, Liu G, Abrao M, Smart N, Heniford T. Perspectives on surgery in the time of COVID-19: Safety first. J Minim Invasive Gynecol 2020;27(4):792–3. [CrossRef]
[Pubmed]

27.
Ross SW, Lauer CW, Miles WS, et al. Maximizing the calm before the storm: Tiered surgical response plan for novel coronavirus (COVID-19). J Am Coll Surg 2020;230(6):1080–91.e3. [CrossRef]
[Pubmed]

28.
Sibony AL. The UK COVID-19 Response: A Behavioural Irony? European Journal of Risk Regulation 2020;11(2):350–7. [CrossRef]

29.
Xiang YT, Jin Y, Wang Y, Zhang Q, Zhang L, Cheung T. Tribute to health workers in China: A group of respectable population during the outbreak of the COVID-19. Int J Biol Sci 2020;16(10):1739–40. [CrossRef]
[Pubmed]

30.
Lei S, Jiang F, Su W, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine 2020;21:100331. [CrossRef]
[Pubmed]

31.
Kimmig R, Verheijen RHM, Rudnicki M, for SERGS Council. Robot assisted surgery during the COVID-19 pandemic, especially for gynecological cancer: A statement of the Society of European Robotic Gynaecological Surgery (SERGS). J Gynecol Oncol 2020;31(3):e59. [CrossRef]
[Pubmed]

32.
Wen X, Li Y. Anesthesia procedure of emergency operation for patients with suspected or confirmed COVID-19. Surg Infect (Larchmt) 2020;21(3):299. [CrossRef]
[Pubmed]

33.
Naspro R, Da Pozzo LF. Urology in the time of corona. Nat Rev Urol 2020;17(5):251–3. [CrossRef]
[Pubmed]

34.
COVIDSurg Collaborative. Global guidance for surgical care during the COVID-19 pandemic. Br J Surg 2020. [CrossRef]
[Pubmed]

35.
Huang J, Hu Y, Wang J, et al. Recommendation about the perioperative prevention of infection to healthcare workers and the anesthesia management of children with SARS-CoV-2 infection. World Jnl Ped Surgery 2020;3(1):e000126. [CrossRef]

36.
Stahel PF. How to risk-stratify elective surgery during the COVID-19 pandemic? Patient Saf Surg 2020;14:8. [CrossRef]
[Pubmed]

37.
Aminian A, Safari S, Razeghian-Jahromi A, Ghorbani M, Delaney CP. COVID-19 outbreak and surgical practice: Unexpected fatality in perioperative period. Ann Surg 2020. [CrossRef]
[Pubmed]

38.
Brücher BLDM, Nigri G, Tinelli A, et al. COVID-19: Pandemic surgery guidance. 4open 2020;3(1):19. [CrossRef]

39.
Mowbray NG, Ansell J, Horwood J, et al. Safe management of surgical smoke in the age of COVID-19. Br J Surg 2020. [CrossRef]
[Pubmed]

40.
Francis N, Dort J, Cho E, et al. SAGES and EAES recommendations for minimally invasive surgery during COVID-19 pandemic. Surg Endosc 2020;34(6):2327–31. [CrossRef]
[Pubmed]

41.
de Leeuw RA, Burger NB, Ceccaroni M, et al. COVID-19 and laparoscopic surgery, a scoping review of current literature and local expertise. JMIR Public Health Surveill 2020. [CrossRef]
[Pubmed]

42.
Balakrishnan K, Schechtman S, Hogikyan ND, Teoh AYB, McGrath B, Brenner MJ. COVID-19 pandemic: What every otolaryngologist-head and neck surgeon needs to know for safe airway management. Otolaryngol Head Neck Surg 2020;162(6):804–8. [CrossRef]
[Pubmed]

43.
Ti LK, Ang LS, Foong TW, Ng BSW. What we do when a COVID-19 patient needs an operation: Operating room preparation and guidance. Can J Anaesth 2020;67(6):756–8. [CrossRef]
[Pubmed]

44.
Coccolini F, Perrone G, Chiarugi M, et al. Surgery in COVID-19 patients: Operational directives. World J Emerg Surg 2020;15(1):25. [CrossRef]
[Pubmed]

45.
Update intercollegiate general surgery guidance on COVID19. [Available at: https://www.rcseng.ac.uk/coronavirus/joint-guidance-for-surgeons-v2/]

46.
Rodrigues-Pinto R, Sousa R, Oliveira A. Preparing to perform trauma and orthopaedic surgery on patients with COVID-19. J Bone Joint Surg Am 2020;102(11):946–50. [CrossRef]
[Pubmed]

47.
Tay JK, Khoo MLC, Loh WS. Surgical considerations for tracheostomy during the COVID-19 pandemic: Lessons learned from the severe acute respiratory syndrome outbreak. JAMA Otolaryngol Head Neck Surg 2020. [CrossRef]
[Pubmed]

48.
49.
Li CI, Pai JY, Chen CH. Characterization of smoke generated during the use of surgical knife in laparotomy surgeries. J Air Waste Manag Assoc 2020;70(3):324–32. [CrossRef]
[Pubmed]

50.
Ansarin M. Surgical management of head and neck tumours during the SARS-CoV (Covid-19) pandemic. Acta Otorhinolaryngol Ital 2020;40(2):87–9. [CrossRef]
[Pubmed]

51.
Emile SH. Should we continue using laparoscopy amid the COVID-19 pandemic? Br J Surg 2020. [CrossRef]
[Pubmed]

52.
Lai YY, Chang CM. A carton-made protective shield for suspicious/confirmed COVID-19 intubation and extubation during surgery. Anesth Analg 2020. [CrossRef]
[Pubmed]

53.
Delgado D, Wyss Quintana F, Perez G, et al. Personal safety during the COVID-19 pandemic: Realities and perspectives of healthcare workers in Latin America. Int J Environ Res Public Health 2020;17(8):2798. [CrossRef]
[Pubmed]

54.
Li W, Zhang J, Xiao S, Sun L. Characteristics of death amongst health worker in China during the outbreak of COVID-19 infection. J Infect 2020;S0163–4453(20):30158–4.
[Pubmed]

55.
Sterpetti AV. Lessons learned during the COVID-19 virus pandemic. J Am Coll Surg 2020;230(6):1092–3. [CrossRef]
[Pubmed]

56.
Vigneswaran Y, Prachand VN, Posner MC, Matthews JB, Hussain M. What is the appropriate use of laparoscopy over open procedures in the current COVID-19 climate? J Gastrointest Surg 2020;1–6. [CrossRef]
[Pubmed]

57.
Aslam S, Mehra MR. COVID-19: Yet another coronavirus challenge in transplantation. J Heart Lung Transplant 2020;39(5):408–9. [CrossRef]
[Pubmed]

58.
Angelico R, Trapani S, Manzia TM, Lombardini L, Tisone G, Cardillo M. The COVIDâ€19 outbreak in Italy: Initial implications for organ transplantation programs. Am J Transplant 2020. [CrossRef]
[Pubmed]

59.
Fix OK, Hameed B, Fontana RJ, et al. Clinical best practice advice for hepatology and liver transplant providers during the COVID-19 pandemic: AASLD expert panel consensus statement. Hepatology 2020. [CrossRef]
[Pubmed]

60.
COVID-19 (coronavirus): FAQs for organ donation and transplantation. 2020. [Available at: https://www.myast.org/sites/default/files/COVID19%20FAQ%20Tx%20Centers%202020.03.11_FINAL.pdf]

SUPPORTING INFORMATION
Author Contributions
Olubunmi Emmanuel Odeyemi - Substantial contributions to conception and design, Acquisition of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
James Oluwadara Eyitayo - Acquisition of data, Interpretation of data, Revising it critically for important intellectual content, Final approval of the version to be published
Emmanuel Moyinolu Oyesiji - Acquisition of data, Revising it critically for important intellectual content, Final approval of the version to be published
Mosi Balogun - Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2020 Olubunmi Emmanuel Odeyemi et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.