|
Case Report
Diaphragmatic eventration in COVID-19 patient: A case report
1 Attending Surgeon, Department of General Surgery at Hospital IESS Quito Sur Quito-Ecuador & Universidad Internacional del Ecuador, Quito, Ecuador
2 Attending Surgeon, Department of General Surgery at Hospital IESS Quito Sur Quito-Ecuador, Quito, Ecuador
3 Chief of General Surgery, Department of General Surgery at Hospital IESS Quito Sur Quito-Ecuador, Quito, Ecuador
4 Resident, Department of Internal Medicine at Hospital IESS Quito Sur Quito- Ecuador, Quito, Ecuador
5 Attending Surgeon at Hospital Vozandes Quito, Quito, Ecuador
6 Resident, Department of Internal Medicine at Hospital IESS Quito Sur Quito-Ecuador, Quito, Ecuador
Address correspondence to:
Gabriel A Molina
Attending Surgeon, Department of General Surgery at Hospital IESS Quito Sur Quito-Ecuador, Quito,
Ecuador
Message to Corresponding Author
Article ID: 100048S05GM2020
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Molina GA, Fuentes G, Herrera JM, Jiménez GE, Ayala AV, Uzcategui MI, Negrete JR, Galarza AJ. Diaphragmatic eventration in COVID-19 patient: A case report. Edorium J Surg 2020;7:100048S05GM2020.ABSTRACT
Introduction: Diaphragmatic eventration is a rare pathology that can potentially affect respiratory functions. They are usually asymptomatic and discovered as an incidental finding; however, in critically ill patients, the lack of respiratory effort could create respiratory difficulties. As the COVID-19 pandemic continues, more people will require mechanical ventilation, developing more diaphragmatic complications. The full extent of this pandemic, including dilemmas, treatment, and long-term complications, will only be available if close follow-up is conducted.
Case Report: We present the case of a 69-year-old female patient; a diaphragmatic eventration was discovered during her stay in the intensive care unit (ICU). Thankfully she completely recovered and on follow-ups are doing well.
Conclusion: Oxygen therapy in patients with severe COVID-19 saves lives, many will need mechanical ventilation, and more and more patients will develop diaphragmatic dysfunction as a side effect of this therapy. The long-term effects of this pandemic are yet to be discovered, nonetheless close follow-up will be essential to reveal the real nature of this disease, its treatment, and complications.
Keywords: COVID-19, Diaphragmatic eventration, Mechanical ventilation
INTRODUCTION
Diaphragmatic weakness is highly prevalent in the ICU patient population [1],[2]. It can lead to significant respiratory complications and a cause of failure to wean off patients from mechanical ventilation successfully [2]. Due to the COVID-19 patients, the need for mechanical ventilators and ICU beds continues to rise [3]. Therefore, more diaphragmatic complications are expected to happen, including diaphragmatic dysfunction, eventration, weakness, and diaphragmatic paralysis [1],[4]. The long-term complications are still unknown; however, close follow-up and prompt treatment of complications will improve these critically ill patients’ outcomes. We present the case of a 69-year-old female patient with COVID-19; a diaphragmatic eventration was discovered during her stay in the ICU. After treatment, she completely recovered and is doing well on follow-ups.
CASE REPORT
The patient is a 69-year-old female with a past medical history of poorly controlled diabetes and hypertension. She presented to the emergency room with a 6-day history of dry cough, fever, and asthenia. At first, the cough was mild; nonetheless, in the last 24 hours, her cough became more severe, and shortness of breath appeared. Therefore, she was brought immediately to the emergency room. On arrival, a tachypneic and confused patient was encountered, her breath sounds were diminished, and her oxygen saturation was below 70%. She was admitted, and high flow oxygen through a face mask was initiated. Complementary exams were requested. A chest computed tomography (CT) revealed a 45% pulmonary compromise with widespread bilateral ground-glass opacities with a posterior predominance. Arterial blood gas reported severe hypoxemia and hypercapnia, and the reverse transcription-polymerase chain reaction (RT-PCR) for the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) test was positive. She was admitted due to acute respiratory distress syndrome (ARDS); however, she continued to deteriorate despite aggressive treatment. Thus intubation, along with mechanical ventilation, was needed.
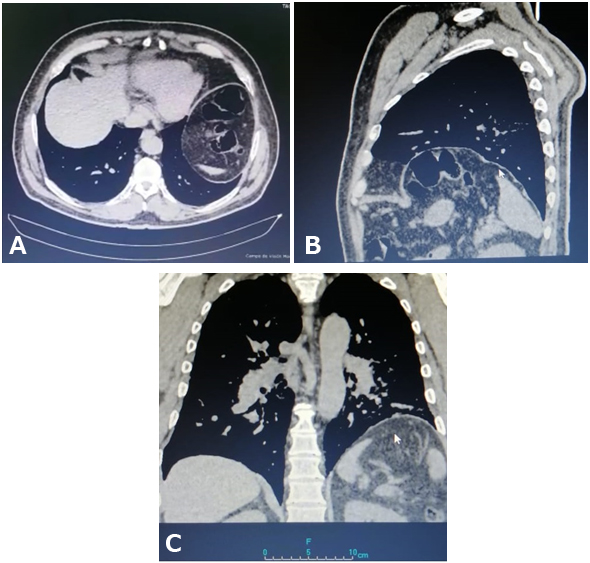
She improved considerably during her stay (21 days) in the ICU. Yet, as the neuromuscular blockade was weaned off, her respiratory effort was insufficient, and a new blockade was needed. A new chest CT was requested, revealing a left-sided diaphragmatic eventration (Figure 1A, Figure 1B, Figure 1C); a latter fluoroscopic assessment of diaphragmatic function showed the paradoxical motion of the elevated hemidiaphragm. Ventilator-induced diaphragmatic dysfunction with left diaphragmatic eventration was suspected. Surgical consultation was needed. Nonetheless, as the patient’s condition improved and successful extubation was achieved with a pressure support ventilation system two days later, she remained under close surveillance until she was discharged.
On follow-ups three months later, dyspnea on exertion remained. A new chest CT showed decreased ground-glass opacities in the right lung with a typical diaphragm.
We associated her dyspnea to the COVID-19 infection, and it has improved considerably with respiratory physiotherapy.
DISCUSSION
The diaphragm is the primary respiratory muscle [1]. Any disease that interferes with the diaphragmatic contraction, innervation, or mechanical functions can cause respiratory dysfunction [1],[2]. Diaphragmatic dysfunction can include eventration, weakness, and diaphragmatic paralysis. Petit et al. were the first to report diaphragm eventration in 1774 [1],[4]. It is a condition in which the left or right diaphragm ascends abnormally high into the chest (more than 2 cm elevation compared to the contralateral side) [2],[5]. “True” diaphragmatic eventration (<0.05% of the adult population) is a congenital defect that affects the muscular portion of the diaphragm [1],[2],[4].
In contrast, eventration in the setting of diaphragmatic dysfunction is an acquired condition. Depending on the cause, this disorder can be unilateral, bilateral, temporary, or permanent [4]. The physiopathology is not yet fully understood; however, many alterations can cause diaphragmatic dysfunction, and the anatomical involvement will determine the dysfunction’s severity. (Brain, central nervous system, spinal cord, brachial plexus, phrenic nerve, lung, and the diaphragmatic muscle itself) [1],[5]. In severely ill patients with mechanical ventilation, it is believed that diaphragmatic dysfunction can be traced to a defect in the mitochondrial reactive oxygen production caused by the abolished diaphragmatic effort; nonetheless, the cellular and molecular pathways are still under study [1],[2].
Patients are usually asymptomatic and discovered incidentally on a chest X-ray. The patients typically become symptomatic in adulthood as they gain weight or suffer a change in lung or chest wall compliance [1],[2],[5]. The difficulty with diaphragmatic eventration is that patients may not have the diaphragm’s natural movement necessary for correct inspiration [2],[5]. Diaphragmatic movement can be diminished, absent, or even paradoxical. As a result, ventilation and perfusion to the lung’s basal portion will be reduced [5],[6]. We believe this is what happened to our patient. As we tried to remove mechanical ventilation, the patient resumed the usual repository effort, and the diaphragm was unable to provide adequate inspiration.
The timing and duration of intubation are yet to be determined; however, in patients with severe COVID-19, oxygen therapy saves lives [3],[7]. Therefore, our patient was placed under mechanical ventilation. Diagnosis should be based on careful history (progression of dyspnea and orthopnea) and physical examination. Nonetheless, imaging studies aid in the diagnosis [1],[5]. Chest X-ray, fluoroscopic test, ultrasound, CT, and phrenic nerve stimulation can be useful to diagnose this pathology correctly [4] as we did in our patient.
Treatment will depend on each patient’s cause and symptomatology; reversible processes must be treated (infection, obesity, metabolic disorders, paraneoplastic, and diabetic). After these pathologies are resolved, the diaphragmatic function can improve up to 40–60% [2],[5]. Therefore, an observation period is necessary before surgery (plication operations should be used for high-level diaphragm eventrations, which results in mediastinal shift) [1],[8]. In more severe cases, a pacemaker or ventilatory support may be needed [2].
Recently published case series showed that length of stay in the ICU and mechanical ventilation duration in severe cases of COVID-19 were almost always more than seven days. This leads to increased exposure to the ICU environment, mechanical ventilation, and prolonged use of neuromuscular blocking, making weaning particularly challenging and increasing the risk of ventilation-induced diaphragm dysfunction [9]. As our patient experienced, the eventration was identified as in incidental finding in a COVID-19 patient under mechanical ventilation, thankfully, the patient recovered, and no surgery was needed.
The COVID-19 pandemic has strained medical systems over the edge. As the disease progresses, better treatment and newer complications are expected to happen. Our understanding of this disease is far from ideal, and we have seen how medications such as hydroxychloroquine, antivirals, and antibiotics have not worked. Since oxygen therapy in patients with severe COVID-19 saves lives, many will need mechanical ventilation, and more and more patients will develop diaphragmatic dysfunction as a side effect of this therapy. The long-term effects of this pandemic are yet to be discovered, nonetheless, close follow-up will be essential to reveal the real nature of this disease, its treatment, and complications.
CONCLUSION
The COVID-19 pandemic has strained medical systems over the edge. As the disease progresses, better treatment and newer complications are expected to happen. Our understanding of this disease is far from ideal, and we have seen how medications such as hydroxychloroquine, antivirals, and antibiotics have not worked. Since oxygen therapy in patients with severe COVID-19 saves lives, many will need mechanical ventilation, and more and more patients will develop diaphragmatic dysfunction as a side effect of this therapy. The long-term effects of this pandemic are yet to be discovered, nonetheless, close follow-up will be essential to reveal the real nature of this disease, its treatment, and complications.
REFERENCES
1.
Ricoy J, RodrÃguez-Núñez N, Ãlvarez-Dobaño JM, Toubes ME, Riveiro V, Valdés L. Diaphragmatic dysfunction. Pulmonology 2019;25(4):223–35. [CrossRef]
[Pubmed]

2.
Groth SS, Andrade RS. Diaphragmatic eventration. Thorac Surg Clin 2009;19(4):511–9. [CrossRef]
[Pubmed]

3.
Petrof BJ, Hussain SN. Ventilator-induced diaphragmatic dysfunction: What have we learned? Curr Opin Crit Care 2016;22(1):67–72. [CrossRef]
[Pubmed]

4.
Christensen P. Eventration of the diaphragm. Thorax 1959;14(4):311–9. [CrossRef]
[Pubmed]

5.
Podgaetz E, Diaz I, Andrade RS. To sink the lifted: Selection, technique, and result of laparoscopic diaphragmatic plication for paralysis or eventration. Thorac Cardiovasc Surg 2016;64(8):631–40. [CrossRef]
[Pubmed]

6.
Dondorp AM, Hayat M, Aryal D, Beane A, Schultz MJ. Respiratory support in COVID-19 patients, with a focus on resource-limited settings. Am J Trop Med Hyg 2020;102(6):1191–7. [CrossRef]
[Pubmed]

7.
Sartini C, Tresoldi M, Scarpellini P, et al. Respiratory parameters in patients with COVID-19 after using noninvasive ventilation in the prone position outside the intensive care unit. JAMA 2020;323(22):2338–40. [CrossRef]
[Pubmed]

8.
Özkan S, Yazici Ü, Aydin E, Karaoğlanoğlu N. Is surgical plication necessary in diaphragm eventration? Asian J Surg 2016;39(2):59–65. [CrossRef]
[Pubmed]

9.
Guarracino F, Vetrugno L, Forfori F, et al. Lung, heart, vascular, and diaphragm ultrasound examination of COVID-19 patients: A comprehensive approach. J Cardiothorac Vasc Anesth 2020. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Gabriel A Molina - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Germanico Fuentes - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Juan M Herrera - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Galo Enrique Jimén - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Andres Vinicio Ayala - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Maria Isabel Uzcategui - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
José Ricardo Negrete - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Andres Jiménez Galar - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2020 Gabriel A Molina et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.