|
Case Report
A rare presentation of giant gallbladder
1 Department of General Surgery, The EMMS Hospital, Nazareth, Israel
Address correspondence to:
Amir Camil Obeid
Department of General Surgery, The EMMS Hospital, Nazareth,
Israel
Message to Corresponding Author
Article ID: 100058S05AO2022
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Obeid AC, Sayida S, Abboud W. A rare presentation of giant gallbladder. Edorium J Surg 2022;9(2):8–11.ABSTRACT
In common practice enlarged gallbladders are rarely encountered and there are a minimal number of cases reported worldwide. Most of these encounters have been associated with malignancy which is contrary to our finding. We describe a case of chronic cholecystitis which had the rare association of a giant gallbladder which was treated by surgical resection without any pathological associations. The review also describes the different grading of cholecystitis and various management approaches which are applied in common practice. Due to the fact that cases of giant gallbladders are a rare encounter, documenting this case will provide further analysis for future studies.
Keywords: Biliary, Cholecystitis, Gallbladder, Malignancy
INTRODUCTION
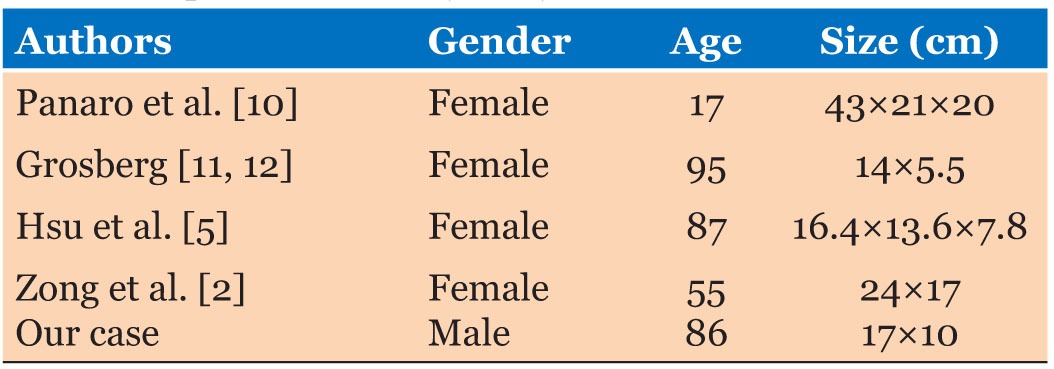
Previously reported cases of giant gallbladder have revealed the association with tumors or gallstones [1],[2]. A minimal amount of giant gallbladder cases has been reported (Table 1). We present a case of a giant gallbladder in a patient with recurrent hospital admissions due to chronic biliary disease.
CASE REPORT
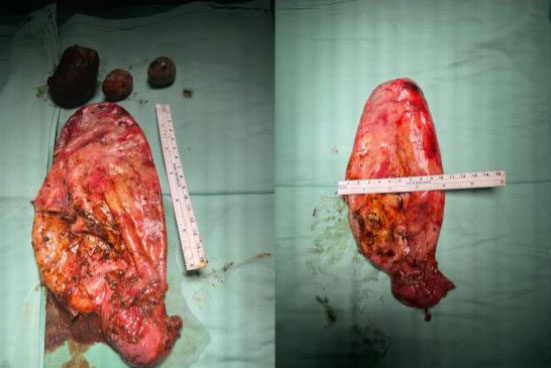
An 87-year-old male with no significant past medical history was admitted twice for biliary disease. The patient’s first admission consisted of a diagnosis of biliary pancreatitis with obstructive jaundice due to biliary stones which was diagnosed upon arrival and underwent ultrasonography (US) which revealed biliary stones and a polyp of 1.5 cm without cholecystitis and the incidental encounter of an oversized gallbladder 17 by 10 cm in length (Figure 1). During his hospital stay the patient developed worsening conditions and underwent emergent endoscopic retrograde cholangiopancreatography (ERCP) which consisted of stone extraction and stent insertion which aided in resolution of the patient’s condition. In addition, the proper treatment was performed by undergoing emergent ERCP due to the association of pancreatitis and a cholecystectomy was not the treatment of choice at the time due to patient comorbidities. A month following the ERCP, the patient was readmitted due to cholecystitis and the oversized gallbladder was reencountered by US, having similar dimensions of 17×10 cm in size. The patient was treated conservatively which consisted of antibiotics, analgesics, and fasting for a few days. Prior to discharge from the hospital the patient began a non-fat diet. The hospital stay concluded without any complications as previously encountered. An elective laparoscopic cholecystectomy was performed a couple of weeks following the prior admission. The surgery was performed laparoscopically without any complications. During the surgical procedure, the gallbladder consisted of an empyema of the sac and was inflamed which was difficult to determine the anatomical structures and its origin in order to perform the necessary procedure. Drainage of the sac was performed prior to continuation of resection due to its large size of 17×10 cm. In addition, the presence of an empyema couldn’t be determined prior to elective surgery which is why our decision of treatment upon the first admission was correctly carried out. As no pathological findings such as a tumor or obstructive manner were observed, the surgery was fulfilled without any complications (Figure 2). There were no post-operative complications and the patient was discharged on the second post-operative day. Pathology results showed signs of chronic cholecystitis without malignant findings.
DISCUSSION
As described enlarged gallbladders are rarely encountered in common practice. The definition of a normal gallbladder length is no larger than 7–10 centimeters (cm) [1],[3].
Several theories are identified which establish the mechanism of enlarged gallbladder.
Few theories state that impacted stones without cholecystitis cause long-standing obstruction resulting in reduced biliary drainage causing the epithelium of the gallbladder to secrete mucus also increasing intraluminal pressure resulting in distention of the gallbladder [1],[4]. Many authors have stated that oversized gallbladder is correlated with pathological states such as malignant tumors of the pancreas or biliary tree [2],[3],[5]. Over the years gallbladder distention has been frequently associated with malignancy. According to Courvoisier’s law, patients with a palpable gallbladder presenting with jaundice are often diagnosed with a malignant obstruction of the common bile duct. Courvoisier et al. also described that dilation of the gallbladder is rare but not only correlated with malignancy but can also be associated with obstructing stones [2],[6]. Further details regarding indications of management in particular situations when dealing with cholecystitis are performed depending on the severity of the disease. Throughout recent years certain guidelines have been established in order to define and treat accordingly. According to the Tokyo guidelines which were established in 2007 and updated in 2013 and recently in 2018, determined and graded the severity of cholecystitis into three grades mild, moderate and severe. Grade I (mild acute cholecystitis) is defined as acute cholecystitis in a patient with no organ dysfunction and limited disease in the gallbladder, making cholecystectomy a low-risk procedure. Grade II (moderate acute cholecystitis) is associated with no organ dysfunction; however, there is an extensive disease in the gallbladder, resulting in increased difficulty in safely performing a cholecystectomy and an increased risk of biliary tract injury during the inflammation-related cholecystectomy surgery. Grade III (severe acute cholecystitis) is defined as acute cholecystitis with organ dysfunction. Depending on the severity of cholecystitis and specific patients such as the elderly, percutaneous cholecystostomy is a method which can be used in elderly patients with cholecystitis in cases where emergency surgery cannot be performed. Infection is controlled by drainage of the gallbladder. After percutaneous cholecystostomy, cholecystectomy can be performed under more appropriate and elective conditions [7],[8],[9].
Our case report is among the few reported cases having an oversized gallbladder and represents gallstones can be associated with unusually large gallbladder. This case accounts for one of the only few gallbladder cases of its size. The relation of giant gallbladder with malignancy is not quite understood which is why there have been few articles/cases to be accounted for in order to support this case. Various cases published have been associated with malignancy although the majority are not. All in all, our case has stated and provided more information about giant gallbladder than any other cases published in today’s literature.
CONCLUSION
Reports of giant gallbladder are rare and very few cases have been published throughout the history of medicine. The pathogenesis remains ongoing research despite advances in surgical medicine. The entity of having an enlarged gallbladder warrants surgical intervention to prevent ongoing inflammatory or malignant processes.
REFERENCES
1.
2.
Zong L, Chen P, Wang L, He C, Wang G, Jiang J, Wang H. A case of congenital giant gallbladder with massive hydrops mimicking celiac cyst. Oncol Lett 2013;5(1):226–8. [CrossRef]
[Pubmed]

3.
Jahantab MB, Salehi V, Mehrabi S, Abedini L, Yavari Barhaghtalab MJ. Cholecystomegaly: A case report and review of the literature. Case Rep Gastrointest Med 2020;2020:8825167. [CrossRef]
[Pubmed]

4.
5.
Hsu KF, Yeh CL, Shih ML, Hsieh CB, Hsu HM. Giant gallbladder: Adenocarcinoma complicated with empyema. J Trauma 2011;70(1):261. [CrossRef]
[Pubmed]

6.
Memon AA, Soomro MI, Soomro QA. Courvoisier’s law revisited. J Coll Physicians Surg Pak 2012;22(6):392–4.
[Pubmed]

7.
Takada T, Strasberg SM, Solomkin JS, et al. TG13: Updated Tokyo Guidelines for the management of acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci 2013;20(1):1–7. [CrossRef]
[Pubmed]

8.
Yokoe M, Hata J, Takada T, et al. Tokyo Guidelines 2018: Diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci 2018;25(1):41–54. [CrossRef]
[Pubmed]

9.
Hirota M, Takada T, Kawarada Y, et al. Diagnostic criteria and severity assessment of acute cholecystitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg 2007;14(1):78–82. [CrossRef]
[Pubmed]

10.
Panaro F, Chastaing L, Navarro F. Education and imaging. Hepatobiliary and pancreatic: Giant gallbladder associated with Byler’s disease. J Gastroenterol Hepatol 2012;27(3):620. [CrossRef]
[Pubmed]

11.
Grosberg SJ. Giant gallbladder. Am J Dig Dis 1962;7:1039–40. [CrossRef]
[Pubmed]

12.
Kuznetsov AV, Borodach AV, Fedin EN, Khromova AD. Giant gallbladder: A case report and review of literature. Int J Surg Case Rep 2014;5(10):673–6. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Amir Camil Obeid - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Sa'd Sayida - Interpretation of data, Revising it critically for important intellectual content, Final approval of the version to be published
Wisam Abboud - Interpretation of data, Revising it critically for important intellectual content, Final approval of the version to be published
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2022 Amir Camil Obeid et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.