|
Research Articles
Tissue adhesive (2-octylcyanoacrylate) versus standard wound closure in patients undergoing breast lump excision
1 General Surgeon, Department of Surgery, University of Abuja Teaching Hospital, Gwagwalada, FCT, Nigeria
2 Consultant Paediatric Surgeon, Department of Surgery, University of Abuja Teaching Hospital, Gwagwalada, FCT, Nigeria
3 Professor of General Surgery, College of Health Sciences, University of Abuja and University of Abuja Teaching Hospital, Gwagwalada, FCT, Nigeria
Address correspondence to:
Umoke Ifeanyi Charles
Department of Surgery, University of Abuja Teaching Hospital Gwagwalada, FCT, Abuja,
Nigeria
Message to Corresponding Author
Article ID: 100037S05UC2019
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Umoke IC, Olori S, Garba ES. Tissue adhesive (2-octylcyanoacrylate) versus standard wound closure in patients undergoing breast lump excision. Edorium J Surg 2019;6:100037S05UC2019.ABSTRACT
Aims: Topical 2-octylcyanoacrylate, OCA, is an alternative to traditional devices for closing short surgical incisions. Studies show that the use of OCA for the closure of surgical wounds leads to cosmetic outcome superior to conventional sutures. Only few studies have investigated OCA in breast surgery in our environment. The aim of this study was to compare OCA with vicryl 2.0 in skin wound closure for patients undergoing breast lump excision.
Methods: A prospective randomized controlled study in which 44 patients were randomly allocated to skin closure with vicryl 2.0 or OCA group. Forty-one patients completed the study. The wounds were graded at three months for cosmesis using the Hollander Wound Evaluation Scale, HWES, and the Visual Analogue Scale, VAS, respectively. Wound evaluation scores, ease of wound management, and wound complications were compared for both groups. Results were analyzed using SPSS version 20.0.
Results: There were no differences in the three variables between the two groups. The wound closure time was significantly faster in the OCA group (p<0.001), which also had a significantly shorter duration of time between surgery and taking the first shower (p<0.001), but a higher wound dehiscence rate.
Conclusion: Octylcyanoacrylate offered comparable cosmetic outcome to vicryl 2.0 in the closure of breast wounds following lumpectomy for benign lumps and had a faster wound closure time but a higher wound dehiscence rate.
Keywords: Breast surgery, Tissue adhesives, Wound closure
INTRODUCTION
Breast surgery is commonly performed worldwide. Thousands of patients undergo breast surgeries each year for various indications which range from cosmetic to excision of benign or malignant lesions. In Nigeria, a significant number of patients undergo breast lump surgery each year. Aliet al. [1] in Maiduguri observed that a total of 913 patients averaging 152 per year underwent breast lump excision in a period spanning six years. Yusufu et al. [2] in Zaria reported 428 cases of breast lumps in a 14 year period most of whom underwent excision biopsies for evaluation. Varying but considerable figures were reported in Ibadan by Irabor and Okolo [3], Echojoh et al. [4], and Ochicha et al. [5]. A good number of these patients were young women between the ages of 16 and 35 years.
Thus an important factor for the vast majority of them is the aesthetic result [6]. Precise approximation of skin incision with wound closure devices is critical for a favorable cosmetic, surgical, and functional result. Avoidance of tension on the wound and bringing the edges of the skin together in an everted orientation are key for optimum wound healing and cosmesis [7]. In our environment, suturing is the most common method of wound closure.
Suturing generally is time-consuming, requires specialized instruments, carries the risk of needle stick injury to the practitioner, and may require the patient to come back for suture removal [8]. In addition, if sutures are tied too tightly or left in place for an excessive time, they may leave permanent suture marks which are cosmetically unacceptable [9]. Furthermore, if sutures are removed before adequate healing, the lack of adequate wound tensile strength may result in wound dehiscence or a widened scar.
Surgical site infection also impairs wound healing and leads to ugly scars. The ultimate goal of wound management is to achieve a functional and cosmetically pleasing repair [10]. Ideally, incision closure should be simple, safe, rapid, inexpensive, painless, and result in optimal cosmetic appearance of the scar [11]. The cyanoacrylate tissue adhesive offers many of these characteristics. It is safe, simple, rapid, and painless and results in optimal scar appearance. Supplied as monomers in liquid form, they polymerize on contract with tissue anions, forming a strong bond that holds the apposed wound edges together.
The cyanoacrylate adhesive usually sloughs off within 5–10 days as the wound re-epithelizes. 2-Octycyanoacrylate is a new, improved, formulated cyanoacrylate designed to improve on performance as a tissue adhesive. Some studies have reported a superior cosmetic scar outcome with OCA. However, only few studies have compared the two skin closure techniques in breast surgery in our environment. The purpose of this study, therefore, is to compare the two techniques.
MATERIALS AND METHODS
The study was carried out in University of Abuja Teaching Hospital, Gwagwalada, Nigeria over a period of 12 months from October 2016 to September 2017.
Inclusion criteria
- Consecutive female patients above 16 years of age with breast lump presenting at the surgical outpatient clinic of University of Abuja Teaching Hospital, Gwagwalada who consented to the study were included.
Exclusion criteria
- Patients with known blood-clotting disorders.
- Positive personal or family history of keloid or hypertrophic scar formation.
- Known allergy to cyanoacrylate or formaldehyde.
- Previous operation on the index breast.
Randomization
Forty-one patients (21 in the vicryl 2.0 group and 20 in the OCA group) completed the study. Patients were instructed to randomly pick a number from 1 to 41 (sample size) from a bag containing these numbers which were wrapped to blind patients from the numbers they were choosing. All those who chose odd numbers were allotted to the standard wound closure (SWC) group while those who chose even numbers were allotted to the tissue adhesive (OCA) group. Randomization was done just prior to skin closure to avoid bias in subcutaneous closure to bring wound edges together prior to skin closure.
Procedure
Patients underwent excision biopsies under local anesthesia for their breast lumps using either the circumareolar (Webster) incision for lesions close to the nipple/ areolar area or a radial incision centered on the lump for lesions further away from the nipple/areolar complex. A 4–5 cm incision was used to access the lumps in both groups.
At the end of the surgical procedure, accurate hemostasis was achieved either by the electrocautery or by suture ligation.
For all patients, the total length of subcutaneous sutures (vicryl 2.0) applied to aid the in apposition of the wound margins, relieve tension, ensure adequate skin edge eversion was recorded. Before closure, the breast was cleaned with sterile saline solution and an antiseptic agent. Skin closure was performed based on patient’s group. Randomization was done just prior to skin closure. Patients in the SWC group underwent subcutaneous vicryl 2.0 skin closure. Then a dry dressing was applied. Patient randomized to the OCA group had their wounds closed with the tissue adhesive (DERMABOND by Ethicon US, LLC). The tissue adhesive vial was opened and the adhesive expressed through the tip. The adhesive was then applied over the approximated wound edges which waseverted using tooth forceps. Care was taken not to push the tip of the vial beyond the dermal margin and to apply the adhesive in two coatings to ensure adequate seal. The adhesive was allowed for an average of 55 seconds which was the minimum time required for polymerization to occur.
The length of suture used in the subcutaneous layer for wound edge apposition for each and every wound and the time required for skin closure were recorded for both groups. Patients in the SWC were instructed to keep their wounds clean and dry for at least 48 hours after surgery. The OCA group was permitted to get the wounds wet and to shower starting the same day or the day after the surgical procedure.
All procedures were performed by three senior registrars in the General Surgery Unit. Scar assessments were performed by two senior registrars blinded to the wound closure techniques.
Outcome measures
Duration of wound closure: The time taken to close each wound in both groups were recorded as were the lengths of each incision which were kept between 4 and 5 cm. The duration of closure in the SWC group was recorded from the time of placement of the first to the last stitch, while in the OCA group, it was recorded as the time taken as the application time plus the time required for it to polymerize.
Wound infection: At the fourth postoperative day, the wounds were examined for signs of infection(presence of redness, undue tenderness, and wound discharge with positive culture), wound dehiscence (separation of wound edges), and scarring. Clinical suspicion of surgical site infection was confirmed with laboratory evaluation to isolate the etiological bacterial agent and also determine the sensitivity pattern. Appropriate wound care and systemic antibiotics were commenced as indicated. Wound examination was again carried out on the 14th day for resolution of infection.
Cosmesis: Grading for cosmesis was done three months after surgery using the HWES and the VAS. Pictures for the HWES assessment were taken for all patients using a Microsoft Lumia 550 model phone camera. Each patient was followed up for three months. Wound evaluation for cosmesis was by a Senior Registrar blinded to the method of skin closure who would evaluate for step-off borders, contour irregularities, scar width, edge inversion, excessive inflammation, and overall cosmetic appearance.
Patient satisfaction with wound management: For each patient, a satisfaction score(depicting satisfaction with the scar, ease of wound management, viz. ability to shower the same day of surgery) was obtained at the three-month visit. On a scale of 10, with 6 as mark of for “Satisfied” (score ≥6) and “Not Satisfied” (scores <6).
Completed proforma were pooled and the data therein collated. This was analyzed using the SPSS version 20.0. Data were presented as means (±SD) for continuous variable and proportions for categorical variable. Chi square (χ2) and the student t-test were used to compare means where appropriate.
Cosmetic results were compared in contingency tables using 1-tailed test of association. For the other data the student t-test was used for the comparison of the two groups. Results are presented in tables and charts.
RESULTS
Sixty (60) patients were assessed for eligibility. Fifty (50) patients met the eligibility criteria, six (6) of which opted out of the study. Forty-four (44) patients were enrolled out of which forty-one (41) completed the study with an attrition rate of about 6.8%.
Demographics
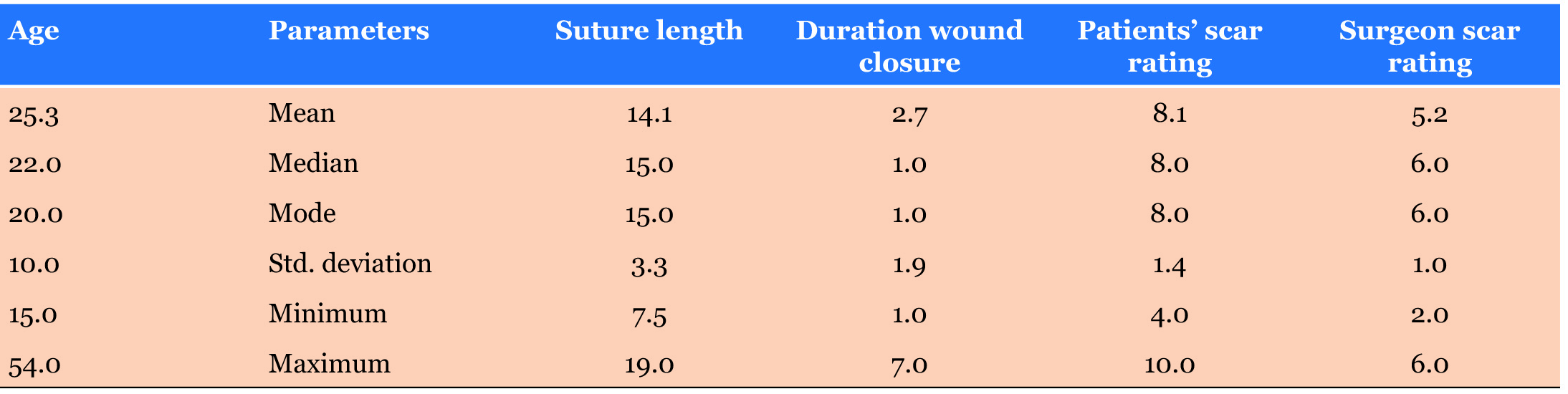
Of the forty-one (41) patients who completed the study, 21 (51.2%) were in the SWC group while 20(48.7%) were in the OCA group. The mean age of the patients was 25.3 years with the age range from 15 to 54 years, the mode was 20 years while the median age was 22 years (Table 1).
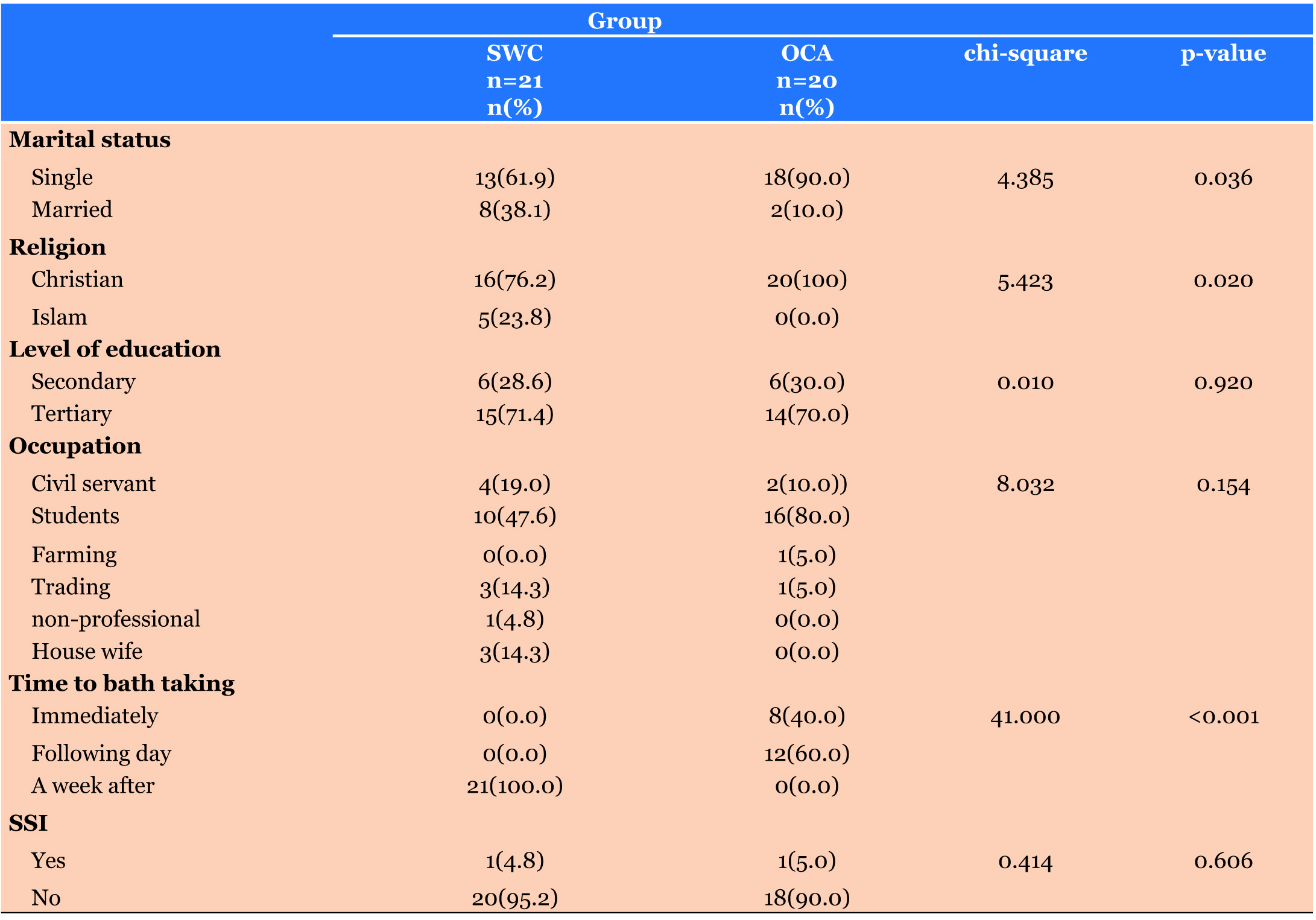
Thirty-one (31) (75.6%) patients were single while 10(24.3%) were married. Students constituted the majority with 26(63.4%) patients while there was only one farmer. Thirty-six (36) (87.8%) patients were Christians while 5 (12.2%) were Moslems (see Table 2).
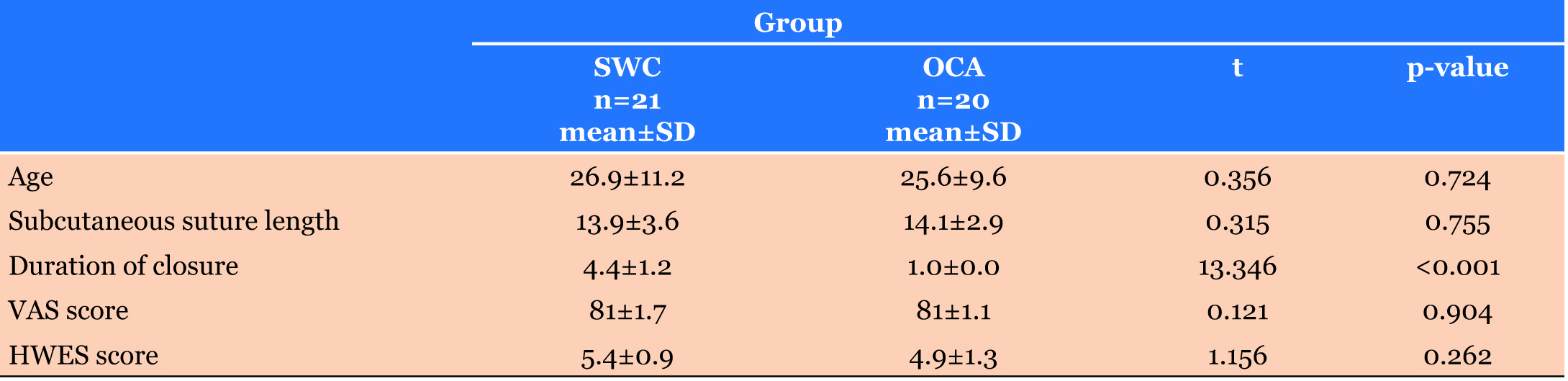
Cosmesis
The mean patients’ scar rating using the VAS was 8.1±1.7 for the SWC group while the mean for the OCA group was 8.1±1.1. There was no statistical significance between these two means with a p-value of 0.904. The mean surgeon’s (blinded) scar rating using the HWES for the SWC group was higher with a value of 5.4±0.9 while the mean for the OCA group was 4.9±1.3 again showing no statistical significance between the two groups with a p-value of 0.262.
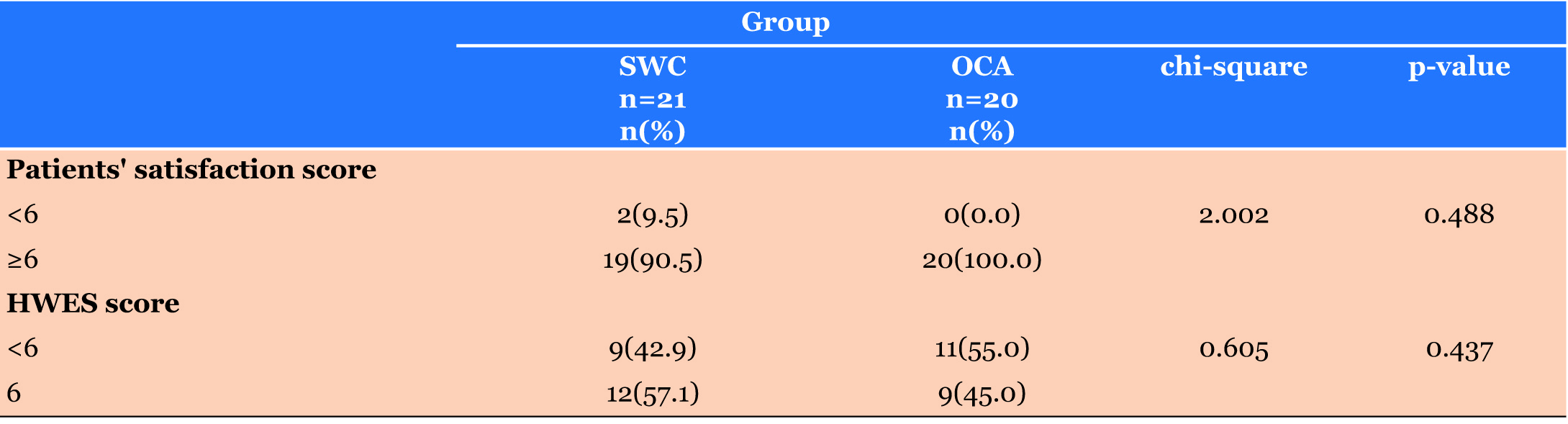
The surgeon’s scar rating was less than optimum(<6) in 9(42.9%) and 11(55%) in the SWC and OCA groups, respectively, while the rating was optimum (6) in 12(57.1%) and 9(45%) in the SWC and OCA groups, respectively. Again there was no statistical significance between the two with a p-value of 0.437 see (Table 3) and (Table 4).
Ease of wound management (patient satisfaction)
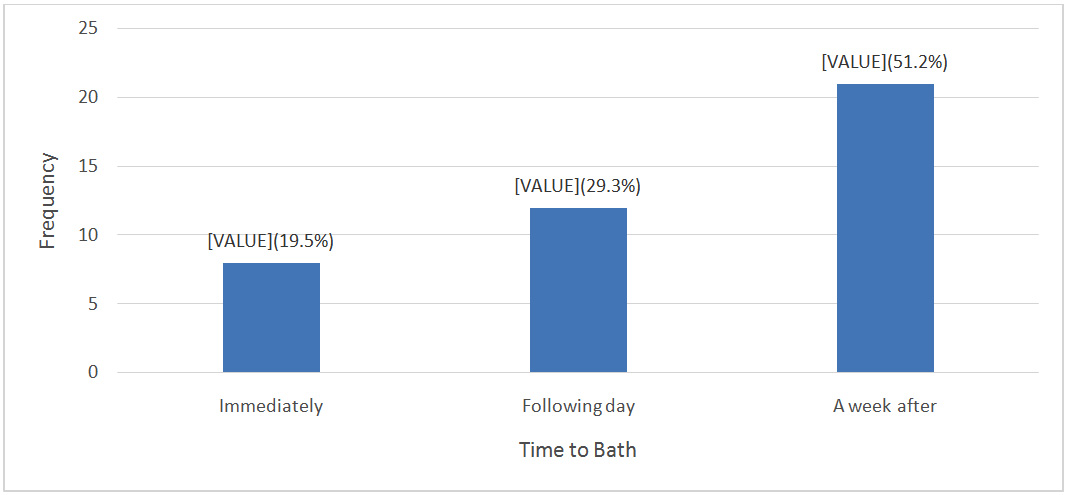
All the 20 patients in the OCA group had their bath between the day of the surgery and the following day while all the 21 patients in the SWC group had their bath on the fourth postoperative day when their wounds were inspected and dressings taken off see (Figure 1).
On a scale of 10, with 6 as the cut off between “Not satisfied” (score of <6) and “Satisfied”(score of ≥6)with the ease of wound management, 2(9.5%)patients in the SWC group were not satisfied with the ease of wound management having to wait for four days to bath after surgery while 19(90.5%) patients were satisfied with the ease of wound management. In the OCA group, all 20(100%) patients were satisfied with the ease of wound management. However, there were no statistical significance between the two groups with a p-value of 0.488 (Table 4).
Time of wound closure
The mean duration of skin closure for the SWC group was 4.4±1.2 minutes while the mean for the OCA group was 1.0±0.0 minutes. The difference was statistically significant with a p-value of <0·001 (Table 3).
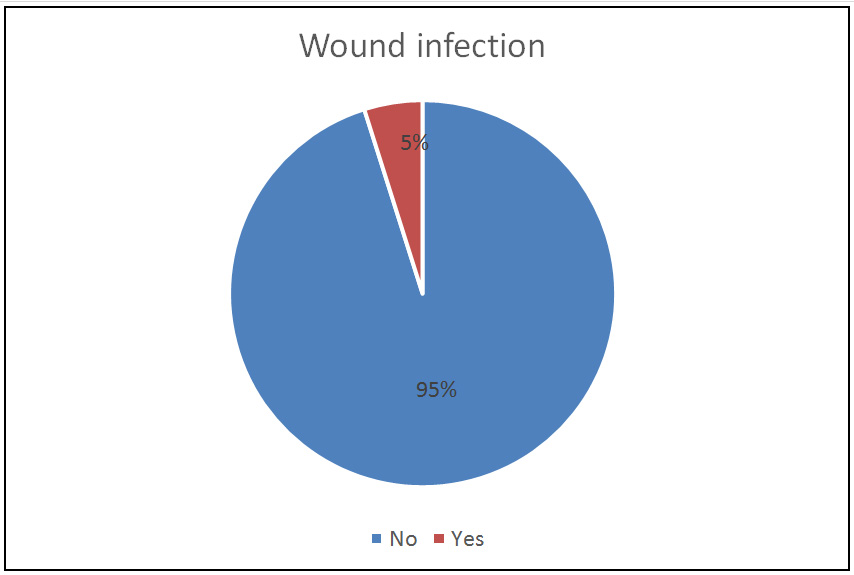
Wound infection
In 1(4.8%) patient in the SWC group and 1(5%) patient in the OCA group developed surgical site infection, SSI, giving a wound infection rate of 5% see (Figure 2). This was not statistically significant with a p-value of 0.606. Staphylococcus aureus was cultured in both cases and patients were treated with antibiotics according to the sensitivity. Wound dehiscence occurred in 2(10%) patients in the OCA group necessitating closure with sutures according to patients’request but none in the SWC group.
Subcuticular suture length
The mean subcuticular suture length for the SWC group was 13.9±3.6cm, while for the OCA group it was 14.1±2.9cm showing no significant difference between the two groups with a p-value of 0.724 see (Table 3).
DISCUSSION
Using the HWES and the VAS there was no statistically significant difference between the OCA and SWC groups in terms of cosmetic outcome. Patients’ satisfaction in terms of ease of wound management was also not statistically significant difference between the two groups. Wounds closed with OCA had a significantly higher HWES score compared with sutures with a p-value of 0.009 [12]. Shivamurthy et al. [13] concluded in their series that both the patients’ and surgeon’s satisfaction scores were higher in the OCA group but, similar to this study, the result was found to be statistically insignificant.
One study found equivalent cosmetic results between OCA and sutured closure [14]. A prospective, randomized, controlled trial conducted by Singer et al. [8] showed that skin closure in traumatic wounds using OCA yielded results that were comparable to SWC with regard to longterm cosmetic outcome. Abhishek et al. [15] observed in their own study that both the OCA and SWC groups showed no significant difference in cosmetic outcome at the three-month follow-up. Chow et al. [16] also found no difference between the two groups for outcomes such as cosmetic appearance and satisfaction in their own series.
Bernard et al. [17], however, observed a statistically significant difference in the blinded VAS cosmesis scores between the two groups with the sutures group scoring higher with a p-value of 0.02. This may have been due to the inclusion of wounds in high tension areas such as the extremities and trunk where OCA may not be able to approximate wound edges adequately leading to widened wound margins and wider scars. The median HWES score was also higher in the suture group though not statistically significant. In a Cochrane review by Dumville et al. [18], the authors reported that there was no significant difference between the two groups in terms of cosmetic outcome, and patients’ as well as operator’s satisfaction.
In this study, it was observed that the OCA group had a faster wound closure time with about a quarter of the time required to close a wound of similar length in the suture group with a p-value of <0·001. Shivamurthy et al. [13] found in their study that it took one-third of the time for wound closure using OCA versus conventional sutures. Sebestra and Bishoff [19] reported that it took an average of 3.7 minutes to close the wound using OCA versus 14 minutes using sutures. Gennari et al. [6] noted that OCA significantly decreased the time required to close breast incisions. Other studies report similar superior speed of application [20],[21],[22].
The SSI rate in this study was 5%. This was slightly higher in the OCA group with a rate of 5% while the rate in the SWC group was 4.7%. This was higher than the findings of Watcher et al. [23] using OCA, for the closure of wounds following spinal surgeries found SSI incidence of 4.3% which was statistically significant when they compared their findings with the SSI incidence in historical controls who had similar surgeries but with suture closure of their surgical wounds. This lower SSI incidence rate may have been due to the use of perioperative prophylactic antibiotics which was not used in this study. Maloney et al. [24] recorded in their own study an overall SSI incidence rate of 8.5%. Maniar and Deshpande [25] and Haider et al. [26] in comparing the two skin closure methods in laparoscopic cholecystectomy found no significant difference in the wound infection rates even though the overall infection rates were higher at 40% and 30%, respectively. This may be due to the wounds being cleanly contaminated.
The wound dehiscence rate for the OCA group was also higher in the findings reported by Chow et al. [16] just like in this study. In a meta-analysis by Dumville et al. [18], most studies reported higher wound dehiscence rates in the OCA group.
The mean age of the patients in this study was 25.3 years. Ali et al. [1] had a similar finding in their study with the mean age of patients with breast lumps (fibroadenoma) at 21±5 years.
CONCLUSION
There is evidence from this study that OCA offered scar cosmetic outcome comparable to vicryl 2.0 in the closure of breast wounds following lumpectomy for benign lumps, and had a faster wound closure time but a higher wound dehiscence rate.
Limitations of the study
- Small sample size. With the small sample size of the study, it is possible that the findings may not be truly representative of a bigger population
- High attrition rate (6.8%). This also contributed to the small sample size which negative impact on the study has been mentioned above.
- The assessment for cosmesis and ease of wound management done at the same time by the patients as well as the use of a nonstandardized scale to assess the patients’ satisfaction may have affected the results of these two outcomes
- The different surgeons involved in the operations may have influenced the outcomes.
Recommendations
- Further studies need to be done in a larger population in order to ascertain the validity of the findings in this study
- Earlier scar/cosmesis assessment to minimize the attrition rate
Further studies to establish a standardized scale for the assessment of patients’ satisfaction.
REFERENCES
1.
Kalfa TA. Warm antibody autoimmune hemolytic anemia. Hematology Am Soc Hematol Educ Program 2016;2016(1):690-7. [CrossRef]

2.
3.
4.
5.
Ochicha O, Edino ST, Mohammed AZ, Amin SN. Benign breast lesions in Kano. Nigerian Journal of Surgical Research 2002;4(1). [CrossRef]

6.
Gennari R, Rotmensz N, Ballardini B, et al. A prospective, randomized, Controlled clinical trial of tissue adhesive (2-Octylcyanoacrylate) versus standard wound closure in breast surgery. Surgery 2004;136(3):593–9. [CrossRef]
[Pubmed]

7.
Davidson TM. Subcutaneous suture placement. Laryngoscope 1987;97(4):501–4. [CrossRef]
[Pubmed]

8.
Singer AJ, Hollander JE, Valentine SM, Turque TW, McCuskey CF, Quinn JV. Prospective, randomized, controlled trial of tissue adhesive (2-octylcyanoacrylate) vs standard wound closure techniques for laceration repair. Stony Brook Octylcyanoacrylate Study Group. Acad Emerg Med 1998;5(2):94–9. [CrossRef]
[Pubmed]

9.
Reiter D. Methods and materials for wound closure. Otolaryngol Clin North Am 1995;28(5):1069–80.
[Pubmed]

10.
Singer AJ, Church AL, Forrestal K, Werblud M, Valentine SM, Hollander JE. Comparision of patient satisfaction and practitioner satisfaction with wound appearance after traumatic wound repair. Acad Emerg Med 1997;4(2):133–7. [CrossRef]
[Pubmed]

11.
Singer AS, Hollander JE, Quinn JV. Evaluation and management of traumatic lacerations. N Engl J Med 1997;337(16):1142–8. [CrossRef]
[Pubmed]

12.
Chen K, Klapper AS, Voige H, Del Priore G. A randomized, controlled study comparing two standardized closure methods of laparoscopic port sites. JSLS 2010;14(3):391–4. [CrossRef]
[Pubmed]

13.
Shivamurthy DM, Singh S, Reddy S. Comparison of octyl-2-cyanoacrylate and conventional sutures in facial skin closure. Natl J Maxillofac Surg 2010;1(1):15–9. [CrossRef]
[Pubmed]

14.
Toriumi DM, O'Grady K, Desai D, Bagal A. Use of octyl-2-cyanoacrylate for skin closure in facial plastic surgery. Plast Reconstr Surg 1998;102(6):2209–19.
[Pubmed]

15.
Soni A, Narula R, Kumar A, Parmar M, Sahore M, Chandel M. Comparing cyanoacrylate tissue adhesive and conventional subcuticular skin sutures for maxillofacial incisions--A prospective randomized trial considering closure time, wound morbidity, and cosmetic outcome. J Oral Maxillofac Surg 2013;71(12):2152.e1–8. [CrossRef]
[Pubmed]

16.
Chow A, Marshall H, Zacharakis E, Paraskeva P, Purkayastha S. Use of tissue glue for surgical incision closure: A systematic review and meta-analysis of randomized controlled trials. J Am Coll Surg 2010;211(1):114–25. [CrossRef]
[Pubmed]

17.
Bernard L, Doyle J, Freidlander SF, Eichenfield LF, Gibbs NF, Cunningham BB. A prospective comparison of octyl cyanoacrylate tissue adhesive (dermabond) and suture for the closure of excisional wounds in children and adolescents. Arch Dermatol 2001;137(9):1177–80.
[Pubmed]

18.
Dumville JC, Coulthard P, Worthington HV, et al. Tissue adhesives for the closure of surgical incisions. Cochrane Database Syst Rev 2014;(11):CD004287. [CrossRef]
[Pubmed]

19.
Sebesta MJ, Bishoff JT. Octylcyanoacrylate skin closure in laparoscopy. J Endourol 2003;17(10):899–903. [CrossRef]
[Pubmed]

20.
Bruns TB, Simon HK, McLario DJ, Sullivan KM, Wood RJ, Anand KJ. Laceration repair using tissue adhesive in a children's emergency department. Pediatrics 1996;98(4 Pt 1):673–5.
[Pubmed]

21.
Elmasalme FN, Matbouli SA, Zuberi MS. Use of tissue adhesive in the closure of small incisions and lacerations. J Pediatr Surg 1995;30(6):837–8. [CrossRef]
[Pubmed]

22.
Applebaum JS, Zalut T, Applebaum D. The use of tissue adhesion for traumatic laceration repair in the emergency department. Ann Emerg Med 1993;22(7):1190–2. [CrossRef]
[Pubmed]

23.
Wachter D, Brückel A, Stein M, Oertel MF, Christophis P, Böker DK. 2-Octyl-cyanoacrylate for wound closure in cervical and lumbar spinal surgery. Neurosurg Rev 2010;33(4):483–9. [CrossRef]
[Pubmed]

24.
Maloney J, Rogers GS, Kapadia M. Surgical corner: A prospective randomized evaluation of cyanoacrylate glue devices in the closure of surgical wounds. J Drugs Dermatol 2013;12(7):810–4.
[Pubmed]

25.
Maniar N, Deshpande AA. A randomized controlled trial of tissue adhesive versus sutures in the closure of port-site incisions in laparoscopic surgery. IOSR Journal Dental and Medical Sciences 2016;15(8):66–70. [CrossRef]

26.
Jan H, Waters N, Haines P, Kent A. LiquiBand® Surgical S topical adhesive versus sutures for the closure of laparoscopic wounds. A randomized controlled trial. Gynecol Surg 2013;10:247–52. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Umoke Ifeanyi Charles - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Olori Samson - Substantial contributions to conception and design, Analysis of data, Revising it critically for important intellectual content, Final approval of the version to be published
Garba E Stephen - Substantial contributions to conception and design, Analysis of data, Revising it critically for important intellectual content, Final approval of the version to be published
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2019 Umoke Ifeanyi Charles et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.