|
Case Report
Lemierre's syndrome, a rare and dangerous condition
1 Department of Surgery, Division of Head and Neck, Hospital Eugenio Espejo, Quito, Ecuador
2 Pontificia Universidad Católica del Ecuador, Department of Surgery, Quito, Ecuador
3 Universidad Central del Ecuador, Department of Surgery, Quito, Ecuador
4 Universidad de lasAméricas, Department of Surgery, Quito, Ecuador
5 PGY2 Resident General Surgery, P.U.C.E, Quito, Ecuador
6 PGY4 Resident General Surgery, P.U.C.E, Quito, Ecuador
Address correspondence to:
Gabriel A Molina
PGY4 Resident General Surgery, P.U.C.E, Quito,
Ecuador
Message to Corresponding Author
Article ID: 100039S05CG2019
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
García CR, Jaramillo KL, Arroyo KA, Muñoz CA, Camacho RB, Pinto PE, Ayala JM, Molina GA. Lemierre’s syndrome, a rare and dangerous condition. Edorium J Surg 2019;6:100039S05CG2019.ABSTRACT
Introduction: Lemierre’s syndrome is a rare and dangerous condition, it usually happens due to the extension of an oropharyngeal infection toward the parapharyngeal space and into the internal jugular vein. This event causes disseminated septic embolism that can be lethal if left untreated. Due to the availability of broad-spectrum antibiotics, its incidence has dramatically decreased in the last few years. Early signs and symptoms are usually vague and a high index of suspicion is required to overcome its morbidity and mortality.
Case Report: We present a case of a 17-year-old male patient, after suffering trauma to his neck, a skin infection appeared that led to cellulitis, abscess, and ultimately internal jugular vein thrombophlebitis. After surgery and antibiotic treatment, the patient recovered successfully.
Conclusion: A high index of suspicion is fundamental in the diagnosis of Lemierre’s syndrome as outcomes are markedly improved when a fast diagnosis is made. Treatment should not be delayed in these severe infections as its complications can cause severe burdens if left untreated.
Keywords: Internal jugular vein, Lemierre’s syndrome, Neck
INTRODUCTION
Lemierre’s syndrome is a rare and near fatal condition, first reported by Courmentand Cade in 1890, and later explained by Andre Lemierre in 1936 [1],[2]. It is usually characterized by an oropharyngeal infection, thrombophlebitis of the internal jugular vein, and metastatic infections due to septic embolus. The incidence of Lemierre’s syndrome has decreased with the introduction of antibiotics in the 1940s, nonetheless, on rare occasions, it can still occur [2],[3]. We present a case of a 17-year-old male patient, who was diagnosed with Lemierre’s syndrome after a skin infection on his neck, thanks to a prompt and aggressive treatment the patient successfully recovered.
CASE REPORT
Patient is an otherwise healthy 17-year-old male without past medical history, he presented to the emergency room with a 15-day history of a growing left neck mass. The mass apparently appeared after a neck and teeth trauma while exercising, nonetheless, he did not find it relevant at that time. At first, the mass was small and well defined, however, during the next few days, it kept growing and was accompanied by pain, edema, and erythema. Twentyfour hours before he sought medical attention, the patient had severe episodes of vomiting, fever, and mild dyspnea. On clinical examination a dehydrated, febrile, and tachycardic patient was encountered, he had a large 10×6 cm mobile, painful, and erythematous mass in the left region of his neck, and was accompanied by edema on his left hemiface. Dental examination revealed swelling and redness around some teeth, and there was a notable diffuse reduction of vesicular murmur in his right lung.
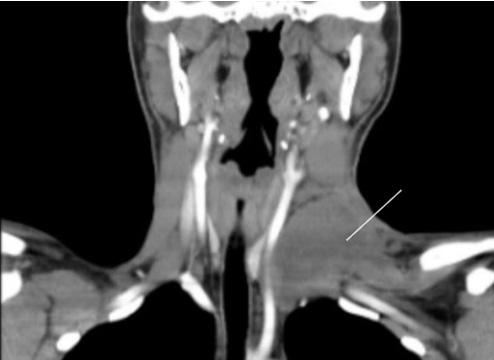
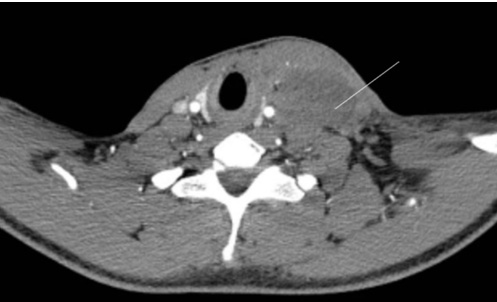
After adequate reanimation complementary exams were requested. Leukocytosis (22,500 mm3), neutrophilia (87%), and elevated C-reactive protein (150 mg/l) were discovered. Due to the size of the mass, a contrastenhanced neck computed tomography (CT) unveiled a 10×6×5 cm inflammatory mass in the left region of his neck, filled with a heterogeneous fluid (Figure 1). There was an increased density and enlargement of soft tissues around the cervical abscess and left hemiface. Thrombophlebitis of the left internal jugular vein was identified as well (Figure 2). A chest x-ray revealed bilateral opacities and a small pleural effusion on his right lung.
With these findings and due to the cervical abscess and clinical condition of the patient, soon after antibiotics were initiated and a left neck incision was done. At surgery, extensive drainage of the pus and necrotic tissue around and within the abscess was completed without complications, and a drain was left in place. Microbiology did not report any microorganisms.
Lemierre’s syndrome was his final diagnosis. His postoperative period was uneventful, after a 10-day scheme of vancomycin and meropenem he was discharged without complications. On follow-up control patient is doing well.
DISCUSSION
Since the description by Andre Lemierre in 1936, the association of oropharyngeal infection with cervical extension, thrombosis of the internal jugular vein, and distant septic emboli has been known as Lemierre’s syndrome [1]. This rare and once lethal infection had a mortality rate up to 90%, nonetheless following the introduction of antibiotics in the 1940s, the incidence of this condition has fallen to a degree that it had been named the “forgotten disease,” with few cases reported in the literature since then [1],[2]. This pathology occurs due to the hematogenous spread of septic embolus from the compromise of the internal jugular vein, in the setting of a bacterial or viral throat infection, yet, odontogenic infections, mastoiditis, parotitis, sinusitis, otitis, infections of the skin, chest, gastrointestinal, or subcutaneous tissues can also be the primary site of contamination [1],[3].
Our patient had a neck and face trauma that could have caused a skin infection that led, to cellulitis, abscess and ultimately internal jugular vein thrombosis.
These septic embolus usually affects the lungs, nonetheless, meningitis, septic arthritis, osteomyelitis, pneumothorax, deep neck infections, liver and spleen abscesses, or even uveitis can happen [2],[4]. Lemierre’s syndrome usually affects young healthy individuals without any age or gender preponderance, due to its rarity (one case per million per year) and broad clinical spectrum it can easily be misdiagnosed [1],[5]. Fusobacterium necrophorumis a gram-negative species of bacteria and a common inhabitant of the human mouth appears to be responsible for this severe infection [5], although other organisms can be implicated including Streptococci group B and C, Streptococcus oralis, Staphylococci, and other Fusobacterium species [2],[6]. In up to 30% of cases, a multi-microbial flora is found, yet, in up to 15% of cases, no organism is identified [2]. As it was found in our patient.
Clinically Lemierre’s syndrome begins in two clinical stages, the initial phase corresponds to an oropharyngeal infection with or without signs of abscess, fever, or cervical lymphadenopathy. While the second phase corresponds to disease spread to the parapharyngeal space with thrombophlebitis of the internal jugular vein and sepsis. At this stage, symptoms depend on the affected organs, however, patients usually present with high fever and chills followed by signs of hemodynamic instability [1],[2],[7]. Diagnosis is based on clinical findings and identifying the thrombosis of the internal jugular vein [2],[3]. Computed tomography (CT) is the most helpful tool although Doppler ultrasound or magnetic resonance can aid in the diagnosis [4],[7],[8]. Management of Lemierre’s syndrome is done with a combination of aggressive intravenous antibiotics and surgical drainage when parapharyngeal, cervical, or mediastinal abscess is detected, ligature of the internal jugular vein is not recommended. Metronidazole, clindamycin, beta-lactam/ beta-lactamase inhibitor combinations, and carbapenems have been successfully used in these infections [9],[10]. Anticoagulation therapy is still debatable as the duration and dosage are not yet defined, although if the thrombosis propagates retrograde and involves the cavernous sinuses of the brain it should be employed [1],[8].
CONCLUSION
A high index of suspicion is fundamental in the diagnosis of Lemierre’s syndrome as outcomes are markedly improved when a fast diagnosis is made. Treatment should not be delayed in these severe infections as its complications can cause severe burdens if left untreated. This case also highlights the awareness that Lemierre’s syndrome can arise from other uncommon causes, and that early signs are regularly subtle and should never be overlooked.
REFERENCES
1.
Lemierre A. On ceriain septicæmias due to anaerobic organisms. The Lancet 1936;227(5874):701–3. [CrossRef]

2.
Karkos PD, Asrani S, Karkos CD, et al. Lemierre's syndrome: A systematic review. Laryngoscope 2009;119(8):1552–9. [CrossRef]
[Pubmed]

3.
Righini CA, Karkas A, Tourniaire R, et al. Lemierre syndrome: Study of 11 cases and literature review. Head Neck 2014;36(7):1044–51. [CrossRef]
[Pubmed]

4.
Risoud M, Mortuaire G, Chevalier D, Rysman B. Atypical Lemierre syndrome. Eur Ann Otorhinolaryngol Head and Neck Dis 2016;133(2):123–4. [CrossRef]
[Pubmed]

5.
Mesrar H, Mesrar J, Maillier B, Kraoua S, Chapoutot L, Delclaux B. Lemierre's syndrome: Diagnosis, exploration, treatment. [Article in French]. Rev Med Interne 2018;39(5):339–45. [CrossRef]
[Pubmed]

6.
Osowicki J, Kapur S, Phuong LK, Dobson S. The long shadow of Lemierre's syndrome. J Infect 2017;74 Suppl 1:S47–53. [CrossRef]
[Pubmed]

7.
Rae J, Misselbrook K. Lemierre’s syndrome – A rare cause of disseminated sepsis requiring multi-organ support. J Intensive Care Soc 2017;18(4):329–33. [CrossRef]
[Pubmed]

8.
Ibrahim J, Noureddin MB, Lootah A, Al Khalidi A, Ghatasheh G, Al Tatari H. A rare case of Lemierre-like syndrome: A case report and literature review. Case Rep Pediatr 2018;2018:9613493. [CrossRef]
[Pubmed]

9.
Bahall M, Giddings S, Bahall K. Lemierre's syndrome: Forgotten, but not absent. BMJ Case Rep 2017;2017. pii: bcr-2017-221203. [CrossRef]
[Pubmed]

10.
Veras RO, Barasuol LL, de Lira CP, et al. Lemierre syndrome: Case report. J Vasc Bras 2018;17(4):337–40. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Cristhian R García - Substantial contributions to conception and design, Drafting the article, Final approval of the version to be published
Katherine Lissette Jaramillo - Substantial contributions to conception and design, Drafting the article, Final approval of the version to be published
Kevin Andres Arroyo - Substantial contributions to conception and design, Acquisition of data, Drafting the article, Final approval of the version to be published
Carmina Alejandra Muñoz - Analysis of data, Interpretation of data, Drafting the article, Final approval of the version to be published
Byron Rodrigo Camacho - Substantial contributions to conception and design, Interpretation of data, Revising it critically for important intellectual content, Final approval of the version to be published
Andrés Esteban Pinto - Substantial contributions to conception and design, Interpretation of data, Drafting the article, Final approval of the version to be published
Jonathan M Ayala - Interpretation of data, Drafting the article, Final approval of the version to be published
Gabriel A Molina - Interpretation of data, Drafting the article, Final approval of the version to be published
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2019 Cristhian R GarcÃa et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.