|
Clinical Studies
Lintula score a fast, easy, and effective tool for acute appendicitis diagnosis
1 General Laparoscopic, Head and Neck Surgeon, Quito Police Hospital N°1, Quito, Ecuador
2 General Laparoscopic and Bariatric Sugeon, Quito Police Hospital N°1, Quito, Ecuador
3 Postgraduate Medical Doctor, PGY4 General Surgery, PUCE, Quito Police Hospital N°1, Quito, Ecuador
Address correspondence to:
Jhony A Delgado
Passage OE9B S12-26 and Los Canelos, Chilibulo, Quito,
Ecuador
Message to Corresponding Author
Article ID: 100046S05AP2020
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Palacios AD, Torres JP, Paredes VH, Delgado JA. Lintula score a fast, easy, and effective tool for acute appendicitis diagnosis. Edorium J Surg 2020;7:100046S05AP2020.ABSTRACT
Aims: To demonstrate the diagnosis accuracy of the Lintula score on acute appendicitis.
Methods: Clinical study not controlled for diagnostic tests validation. Clinical records of 291 patients who experienced an appendectomy between July 2014 and July 2015 were analyzed. Data was transferred to a digital base and it was analyzed in SPSS and R software.
Results: From a total of 291 patients, 262 (86%) had histopathological confirmation. From this group of patients, the majority (60.3%) had a histopathological suppurative type. Lintula score showed 89% sensitivity, 59% specificity, 95% positive predictive value, and 38% negative predictive value with 89% diagnostic precision for the acute appendicitis diagnostic.
Conclusion: Lintula score is a fast and easy-to-perform tool to enable a high diagnostic accuracy for acute appendicitis.
Keywords: Appendicitis, Diagnosis, Lintula score, Sensitivity, Specificity
INTRODUCTION
Approximately, a number of 300,000 people experience appendicectomy each year in the United States. The appendicitis incidence is estimated from 7% to 14% related to sex, life expectancy, and the precision with which the diagnosis is confirmed [1]. Its incidence could be lower in African and Asian countries due to increased protein content in diet [2]. It could happen at any age. However, it tends to be higher in an age group between 10 and 30 years old [3]. It is more common in men rather than in women with a 4:1 ratio [4].
Acute appendicitis is still an important morbidity cause in population as its diagnosis is late or only during diffused advanced peritonitis phases [5].
The goal of this study is to validate the Lintula diagnosis score proposed by Hannu Lintula and collaborators in 2010. This score takes into account nine clinical parameters as signs and symptoms related to illness to diagnose, observe, or discard illness [6].
Some scales are described for appendicitis diagnose. Nevertheless, we focus on the proposal because it does not use laboratory exams nor images as parameters. In fact, Dr. Agrest said “we have arrived at a point where we listened little, we explain less and we ask for many auxiliary tests and we decide on what tests to inform,” losing the relevant anamnesis value and the physical exam [7].
In general, diagnostic studies can cause delay in the definitive management and they associate to complications in the final results [8]. Therefore, the late appendicitis management is associated with prolonged hospitalization, increased risk of perforation (34–75%), surgical wound infection (0–11%), pelvic abscess (1–5%), and late intra-abdominal adhesions [9]. Thus, the need to count on a fast, easy-to-perform, useful, and cost-effective tool for the illness early diagnosis.
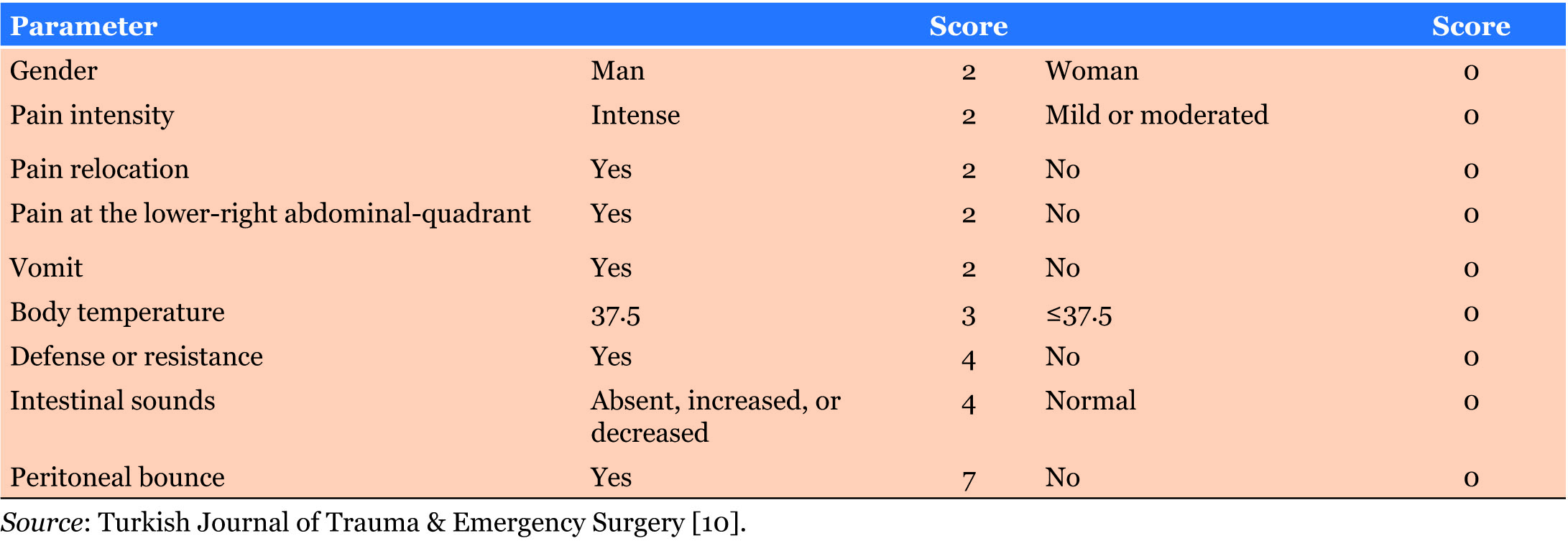
Lintula score includes nine variables as gender, pain intensity, pain relocation, pain at the low right quadrant and vomit. It assigns a minimum score of 0 and a maximum score of 32 points. The prediction cut is ≥21 and the discard cut ≤15. Whereas, patients with score from 16 to 20 are observed [6] as indicated in Table 1.
MATERIALS AND METHODS
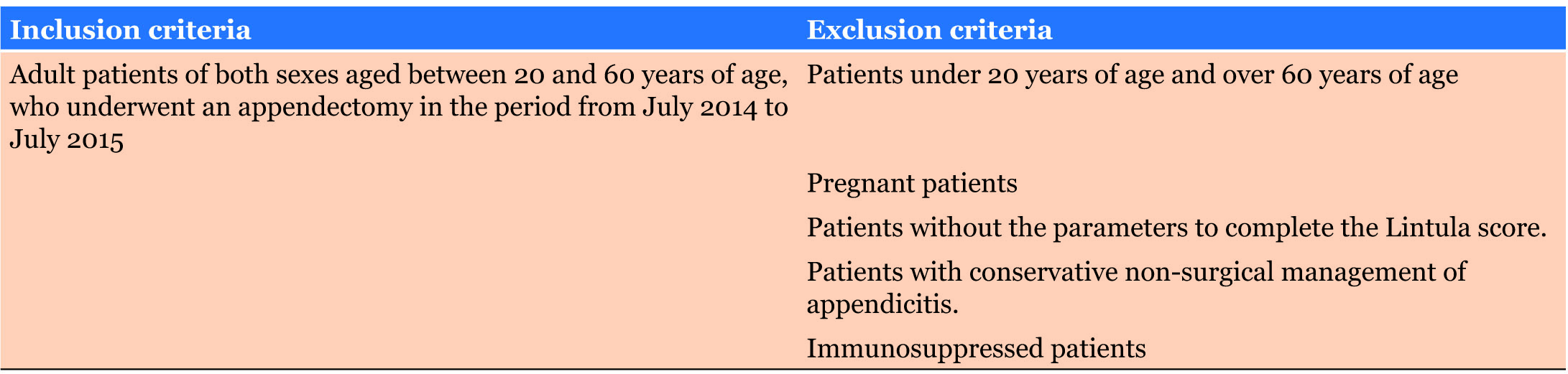
A retrospective study was performed with patients who were diagnosed with acute appendicitis at the San Francisco de Quito Hospital between July 2014 and July 2015 through data collection in clinic records. Furthermore, patients were selected under the inclusion and exclusion criteria (Table 2). Demographic data such as age, sex, ethnic group, co-morbidity presence, previous analgesic usage at the moment of acute appendicitis diagnosis and the histopathologic results were included. The analysis was performed, and results are illustrated in graphics made with SPSS and R statistical packages (2015).
Variable values are reported as average (± standard deviation), mean with its respective interquartile ranges (Q25–Q75), the qualitative variables are reported as percentages. T-student tests were applied to compare or non-parametric tests whether the data did not fit the normality requirement. Discreet variables were compared using Chi-square tests of independence and the exact Fisher test was used if necessary. A sensitivity analysis was performed and a receptor operator curve (ROC) was constructed. The model coefficients of the logistic regression model are reported as odds ratio (OR) with its respective trust intervals. For all comparisons, values lower to 5% were considered significative (p < 0.05).
RESULTS
The sample included a total of 850 patients between July 2014 and July 2015. The size of the sample was calculated with the finite universe formula through which 291 patients were obtained. Then, to select the 291 patients, a random number table was utilized.
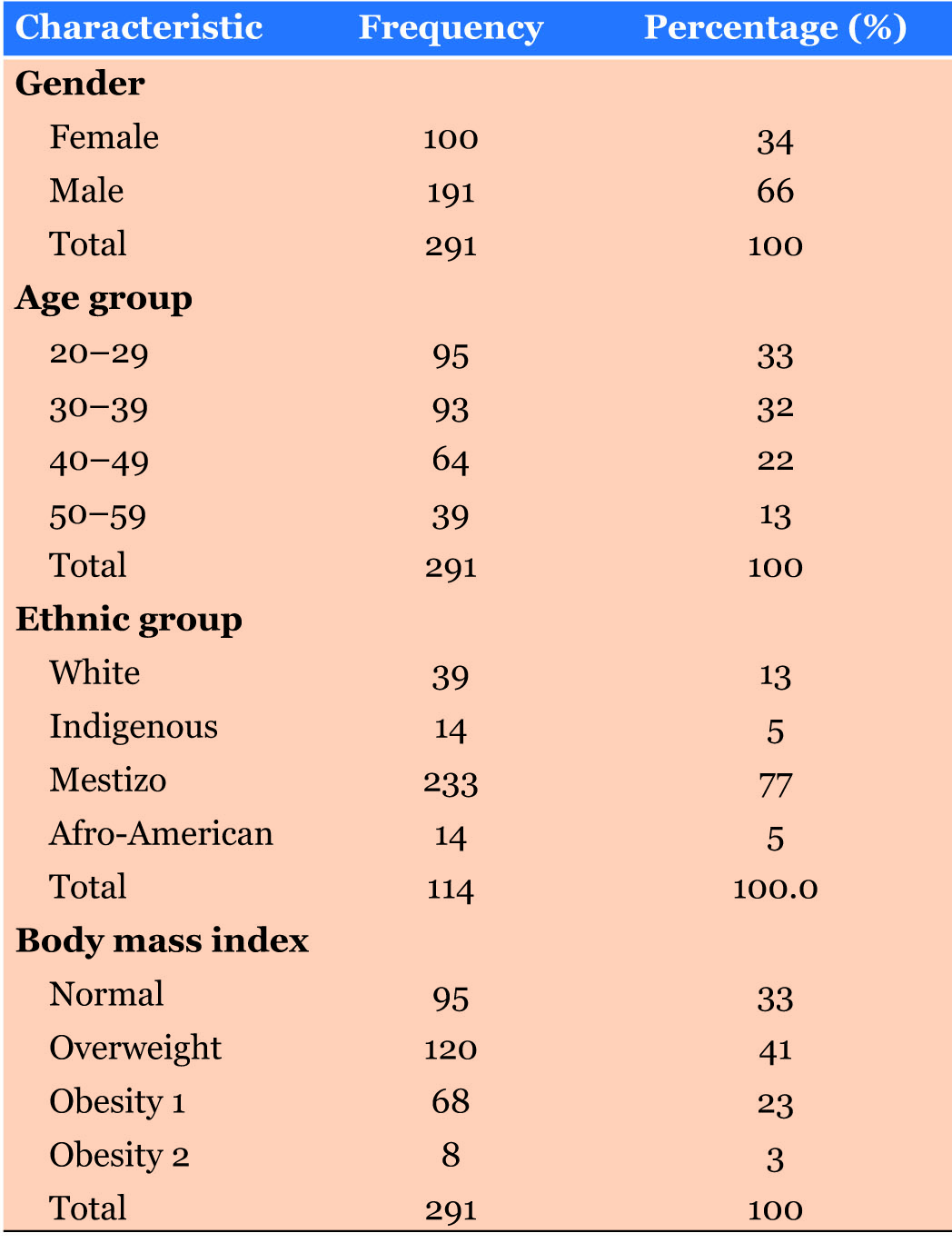
Demographic characteristics
Regarding to sex, a predominant male group was identified. It was represented by 191 patients (66%). Furthermore, contained in this percentage, age was mainly represented by groups between 20–29 and 30–39 years old which correspond to 33% and 32%, respectively. In addition, it was lower in the non-appendicitis group with a difference of less than 4 years [confidence interval (CI) 95%: 0–8 years, p = 0.05]. Moreover, the total body mass index (BMI) did not show differences. Whereas, the ethnic group variable did show predominance in mestizo category represented by 233 patients (77%) (Table 3).
Histopathological confirmation and most frequent operated phase
The sample was constituted by 291 patients with abdominal acute pain who have experienced a surgery as appendicitis was suspected. From this group of patients, a number of 262 had histopathological confirmation (90%). Indeed, the majority of these patients had suppurative histopathologic type (60.3%, n = 158), followed by gangrenous type (25.6%, n = 67), perforated type (11.5%, n = 30) and finally the acute type (2.7%, n = 7).
Lintula score and relation of its scores with the appendicitis phase
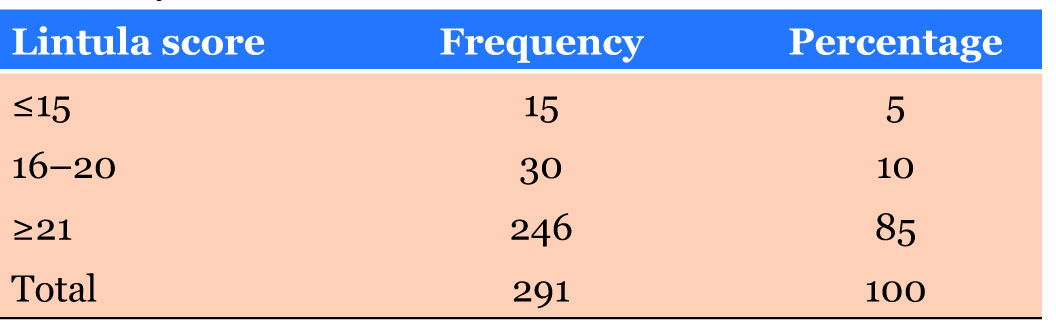
The results showed that from the total of 291 patients who experienced appendectomy, a number of 246 patients (85%) presented a higher or equal value to 21, whereas 30 patients were scored 16 to 21 points (10%), and a number of 15 patients were scored less or equal to 15 (5%) (Table 4).
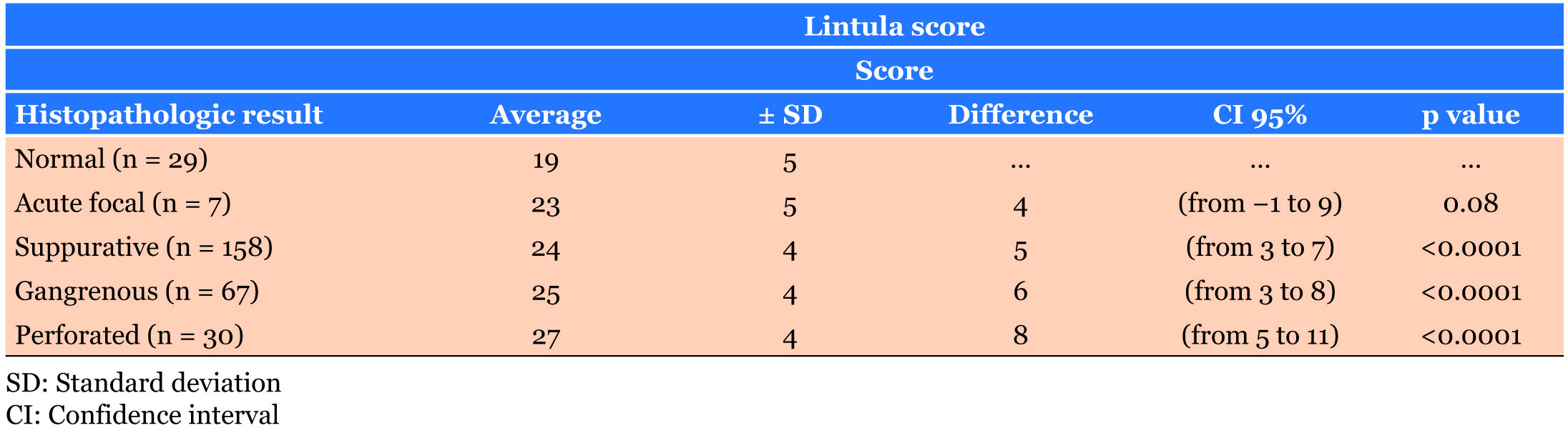
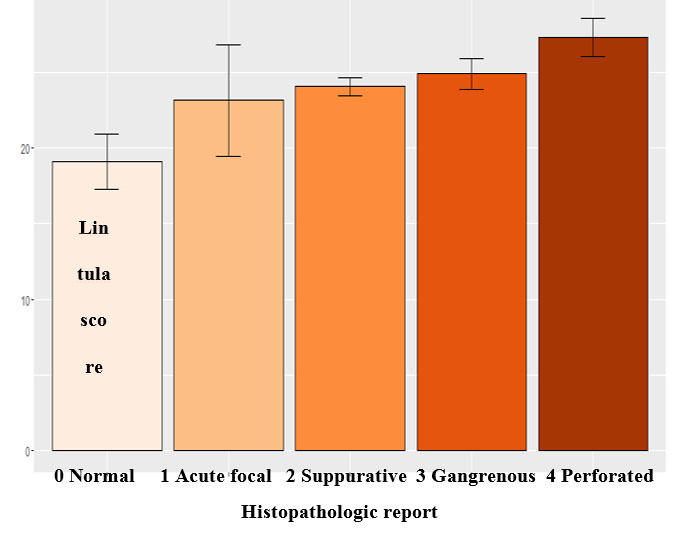
The Lintula score for the non-appendicitis group was 19 points (SD ± 5 points) while the appendicitis group the correspondent score was 25 (SD ± 4 points). Between these groups, the average difference was 6 points (CI 95%: from 7 to 4 points, p < 0.0001). When the group is sorted according to the histopathologic report, a significant difference is noted in the suppurative type (Table 5) (Figure 1).
It is demonstrated that in confirmed patients of appendicitis the Lintula scores were higher, this difference is statistically significant from the suppurative type (p < 0.0001).
Lintula score and its diagnostic values for acute appendicitis
A multivariant model was performed to predict acute appendicitis. The Lintula score was significantly related to diagnosis. This relation was positive, and it determined an increment in the diagnostic probability with an OR: 1.25 (CI 95%: 1.13–1.39; p < 0.0001).
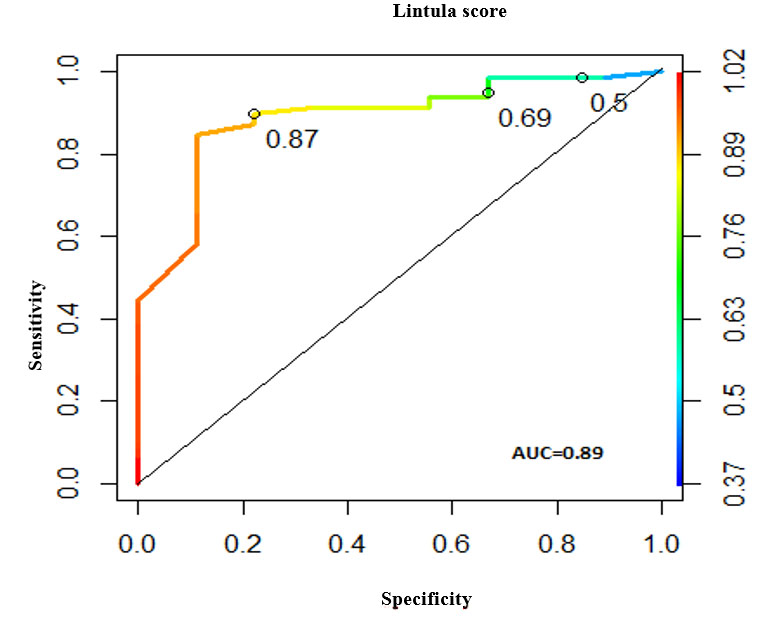
In crossed validation, the Lintula score yielded 92.0%, sensitivity 98.7%, specificity 33.3%, positive predictive value 92.9%, and negative predictive value 75.0%, area under the curve (AUC): 0.89.
The common cut points (Lintula ≥ 16 points and Lintula ≥ 21 points) obtained probabilities of 0.69 and 0.87, respectively. The increment to one cut point with an assigned probability higher or equal to 0.87 (Lintula ≥ 21 points) decreased sensitivity to 89.9%. However, it improved specificity to 77.8% at the expense of false negative increment from 1.3% to 10.1% and decrement of false positives from 66.7% to 22.2%. Indeed, general yield was 89% with an increment of the error general rate from 7.9% to 11.4% (Figure 2).
In addition, AUC was located in 0.89 and the cut points are as indicated in Figure 2. The correspondent probabilities are 0.5 (Lintula ≥ 12 points), 0.69 (Lintula ≥ 16 points), and 0.87 (Lintula ≥ 21 points).
DISCUSSION
Acute appendicitis is the most common pathologic abdominal surgery worldwide. Therefore, in the present study, the authors aim to demonstrate the diagnostic utility of Lintula score for acute appendicitis. As this score only utilizes clinical parameters, we consider validation is important to use this tool.
According to the results, the incidence of presentation corresponds to 1.9:1 in favor of male gender. This data is confirmed by the literature which reports a 1.4:1 relation mainly in male gender rather than in female [11].
Regarding to age, it is reported that the age that mostly presented acute appendicitis was 32 ± 10 years for the histopathologic confirmation group and 36 ± 11 years for the group without histopathologic confirmation. Similar data was reported by Yoldas who found 29.3 ± 10.6 years for the ones who have histopathological confirmation and 33.2 ± 1 year for the group without histopathologic confirmation [9]. The ethnic group showed a noticeable mestizo dominance. However, studies to compare this variable were not found and this data could be attributed to the dominant ethnic group in each region. According to the body mass index (BMI), this variable repeated more frequently in the index between 25 and 29.9 which corresponds to overweigh. In fact, similar data was reported by Lintula et al. (2010) in their validation study [6]. In contrast, this group predominance was not related to the discriminative score value neither it had statistical significance.
It was observed that the majority of patients are diagnosed, and they experience surgery in suppurative phase (63%), this result is comparable to the one obtained by Sanabria et al. (2012) where it is reported that from a total of 206 patients, a percentage of 46.6% experienced surgery in suppurative phase, then, it was the most representative phase [12]. This information is important as it reveals that there is diagnosis and treatment for the pathology during a non-complicated phase.
The authors found that in appendicitis confirmed patients through histopathologic test, the obtained scores were higher. This difference was statistically significant from a suppurative type (p < 0.0001). This data could not be compared due to lack of studies that relate these variables.
Regarding to the yield of the total Lintula score, it is reported a percentage of 89%, with sensitivity of 89%, specificity of 59%, positive predictive value of 95%, and negative predictive value of 38%. These values determine a good yield which is comparable with published data like the one reported by Lintula et al. (2010), where a percentage of 87% was obtained with a specificity of 59–98%, a positive predictive value of 71–98%, and a negative predictive value of 79–86% with a diagnostic precision of 91–92% [6],[9].
The study was retrospectively performed with acute appendicitis diagnosed patients but we believe that it is helpful for the diagnosis. The Lintula score is a very useful tool for doctors who are in rural areas where laboratory tests and imaging facilities are not available, this score helps to manage a transfer to a health care facility with more equipment. The objective of the work is to strengthen a clinic in rural areas of developing countries. The Lintula score may be sufficient for the diagnosis in these mentioned places.
CONCLUSION
Lintula score has a diagnostic accuracy of 89% which catalogs it as a suitable tool to diagnose the illness. The phase that reported more appendicectomies was the suppurative type according to the histopathologic test. Lintula score has a sensibility of 89%, a specificity of 59%, a positive predictive value of 95%, and a negative predictive value of 38%. It is recommended to enhance Lintula score application as a diagnostic tool for acute appendicitis, especially in places where there are rarely diagnostic assistances as laboratories or imaging facilities. The major limitation is that Lintula score has a retrospective character. In addition, it requires a data analysis from a clinic record. Therefore, yield of Lintula score could be improved if a longer period of time study is performed.
REFERENCES
1.
Flum DR. Clinical practice. Acute appendicitis—appendectomy or the “antibiotics first†strategy. N Engl J Med 2015;372(20):1937–43. [CrossRef]
[Pubmed]

2.
Chandrasekaran T, Johnson N. Acute appendicitis. Intestinal surgery II. Surgery (Oxford) 2014;32(8):413–7. [CrossRef]

3.
4.
Humes DJ, Simpson J. Acute appendicitis. BMJ 2006;333(7567):530–4. [CrossRef]
[Pubmed]

5.
Von-Mühlen B, Franzon O, Beduschi MG, Kruel N, Lupselo D. AIR score assessment for acute appendicitis. [Article in Portuguese]. Arq Bras Cir Dig 2015;28(3):171–3. [CrossRef]
[Pubmed]

6.
Lintula H, Kokki H, Pulkkinen J, Kettunen R, Grohn O, Eskelinen M. Diagnostic score in acute appendicitis. Validation of a diagnostic score (Lintula score) for adults with suspected appendicitis. Langenbecks Arch Surg 2010;395(5):495–500. [CrossRef]
[Pubmed]

8.
Ghnnam WM. Elderly versus young patients with appendicitis 3 years experience. Alexandria Journal of Medicine 2012;48(1):9–12. [CrossRef]

9.
Yoldas O, Karaca T, Tez M. External validation of Lintula score in Turkish acute appendicitis patients. Int J Surg 2012;10(1):25–7. [CrossRef]
[Pubmed]

10.
Kırkıl C, Karabulut K, Aygen E, et al. Appendicitis scores may be useful in reducing the costs of treatment for right lower quadrant pain. Ulus Travma Acil Cerrahi Derg 2013;19(1):13–9. [CrossRef]
[Pubmed]

11.
SUPPORTING INFORMATION
Author Contributions
Antonio D Palacios - Substantial contributions to conception and design, Interpretation of data, Drafting the article, Final approval of the version to be published
Juan P Torres - Revising it critically for important intellectual content, Final approval of the version to be published
Victor H Paredes - Acquisition of data, Analysis of data, Revising it critically for important intellectual content, Final approval of the version to be published
Jhony A Delgado - Interpretation of data, Revising it critically for important intellectual content, Final approval of the version to be published
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2020 Antonio D Palacios et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.