|
Research Article
Revisional bariatric surgery: An excellent decision to control reflux and weight regaining
1 General and Laparoscopic Surgeon, Macas General Hospital, Macas, Ecuador
2 General Laparoscopic and Bariatric Surgeon, Quito Police Hospital N°1, Quito, Ecuador
3 General and Laparoscopic Surgeon, Quito Police Hospital N°1, Quito, Ecuador
4 Resident Doctor, General Surgery, General Hospital Macas, Macas, Ecuador
Address correspondence to:
Jhony A Delgado
24 of May and Riobamba, Macas, Morona Santiago,
Ecuador
Message to Corresponding Author
Article ID: 100047S05JD2020
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Delgado JA, Torres JP, Paredes VH, Gordillo AC, Racines GJ, Palacios PA. Revisional bariatric surgery: An excellent decision to control reflux and weight regaining. Edorium J Surg 2020;7:100047S05JD2020.ABSTRACT
Aims: Obesity is currently considered a pandemic and the only treatment that has demonstrated long lasting benefits along time is bariatric surgery. Laparoscopic sleeve gastrectomy (LSG) is the most performed surgery in the world. Nevertheless, its complications such as gastroesophageal reflux and weight gain have led to the conclusion that gastric sleeve to gastric bypass conversion surgery could be an effective alternative to treat them.
Methods: In consensus, the General Surgery service Quito Police Hospital N°1 decides to report the results obtained in the conversion surgeries. These results are obtained from the digital medical record system named Hosvital and from surveys answered by the patients.
Results: A retrospective study was carried out over a 2-year period in which six conversion surgery patients were identified, these patients correspond to 18.75% of the bariatric surgeries performed in this hospital. The majority of these patients (4) are female and the rest (2) are male. Furthermore, the average age was 48 years old. In addition, a significant weight loss was determined by 7.1 months monitoring. The average weight before the surgery was 91 kg. In contrast, the average weight after conversion surgery was 71 kg. Body mass index (BMI) decreased seven points approximately and the excess weight loss percentage (EWLP) increased from 25.06% to 66.6%. Besides, reflux symptoms were solved in 100% of the patients.
Conclusion: Laparoscopic gastric bypass, as a conversion surgery, is an effective treatment to resolve complications as reflux and weight regaining.
Keywords: Bypass, Gastric, Laparoscopic sleeve
INTRODUCTION
Obesity is the body fat excess (cells increase in size and number) in relation to the skinny body fat. According to the World Health Organization (WHO), obesity is a public health problem and it is considered a pandemic. Its prevalence increases and affects to 50% of some country’s population [1]. In children, obesity increases in a worrying manner. In April 2020, WHO announced that over 340 million kids and teenagers aged 5–19 years were reported with overweight and obesity in 2016. Bariatric surgery is the only treatment that has successfully demonstrated weight loss and co-morbidities resolution.
Laparoscopic sleeve gastrectomy has been initially developed as a component of the biliopancreatic derivation with duodenal switch (BPD-DS) surgery that is generally practiced in two stages in super obese patients. It is performed at first stage while biliodigestive derivation is performed at the second stage. When promising results were observed at the first stage of this surgical intervention, LSG was adopted as an individual procedure in 2007. It has been updated and confirmed by Baltasar in 2012 [1],[2]. In recent years, LSG has become the most performed bariatric procedure of the world due to its technical simplicity, acceptable complication incidence, and effective weight loss and co-morbidities resolution without digestive tube integrity modification [3].
Currently, LSG represents 50% of the bariatric procedures performed yearly in the world [4]. However, after 18 months, results are arguable due to weight regaining. In contrast, other studies confirm weight loss maintained until three years after the gastric sleeve surgery [5].
Another cause of LSG conversion is the gastroesophageal reflux disease (GRD) de novo, associated with hiatal hernia. Generally, the candidates for a conversion are patients who have been treated with high doses of proton pump inhibitors (PPI) and symptoms of persistent GRD [1],[6],[7]. The frequency with which the GRD symptoms present de novo after LSG reaches 26% of patients [8].
The Roux-en-Y gastric bypass (RYGB) has been considered as the selection treatment in GRD patients and morbid obesity. This treatment is based on the following reasons: gastric acid reduction, due to the decrease of parietal cells in gastric pouch, bile derivation, and intragastric pressure reduction [9].
Gastric stenosis after LSG has 0.35% incidence, it provokes gastric obstruction, disability to process liquid, solid diet, and vomit. Furthermore, it is considered as a cause of the unsuccessful endoscopic treatments after conversion [3].
Another cause of reintervention is leaking at the staple line reported by Gagner with a 1–5% frequency [6].
Some reports indicate conversion surgery is necessary in 5–11% of the cases as a consequence of LSG failure and RYGB has been proposed as suitable treatment [3].
The aim of this work is to report the results of the conversion surgeries performed at Police Hospital Quito-Ecuador to compare them to the ones reported by other studies.
MATERIALS AND METHODS
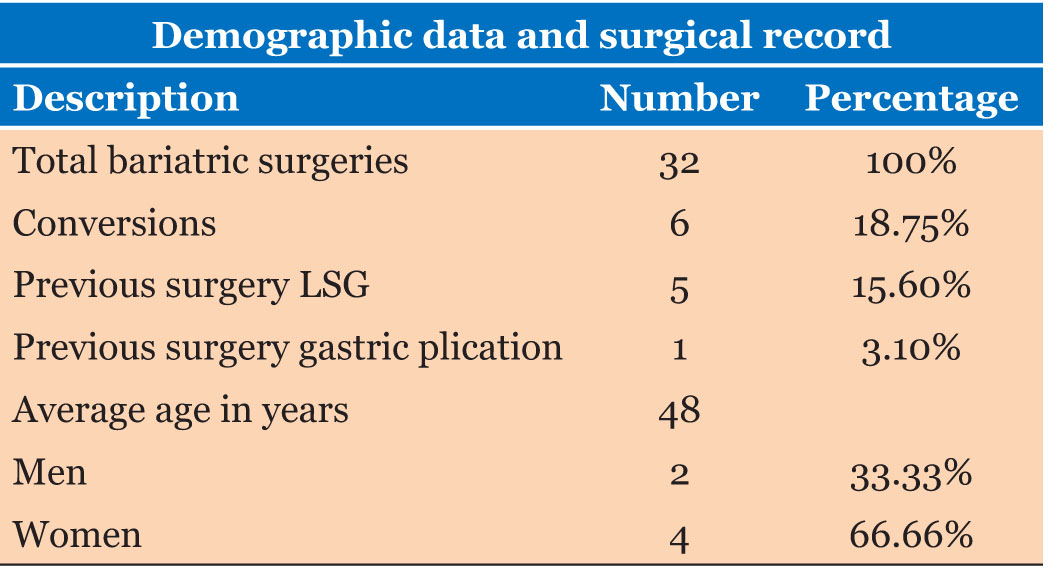
After consensus approval of surgeon doctors of Police Hospital Nº1 Quito, it was decided to perform a retrospective search in the digital medical record system named Hosvital to find conversion cases of LSG or another procedure alternative to RYGB performed in a two year period (2018 and 2019). In this period of time, a number of 32 surgeries were registered LSG and RYGB. Noteworthy, this hospital is not a reference center for bariatric or metabolic surgery. From the mentioned universe, a number of 6 surgeries (18.75%) were RYGB conversions and from these, 5 (15.6%) were preceded by a LSG surgery while 1 surgery (3.1%) was preceded by a laparoscopic gastric intervention. The average time that elapsed between the primary sleeve surgery or gastric application and its conversion to gastric bypass was 58.3 months.
In addition, to obtain more information, the six patients were reached through telephone and a digital survey was completed with previous consent.
RESULTS
From the 6 cases reported as conversions, 3 patients underwent their first surgery at Police Hospital and the rest were intervened in another health center. All conversion surgeries were performed with standard technique in agreement with the institutional criteria.
From the total patients, 4 (66.6%) were women and 2 (33.3%) were men. Patients’ average age was 48 years (Table 1). The average weight, before the first procedure, whether LSG or laparoscopic gastric plication, was 101 kg, corresponding to an average 37.76 kg/m2 BMI. The reasons for medical enquiry to the specialist surgeon were gastroesophageal reflux with endoscopic evaluation that resulted in esophagitis C and one esophagitis B, neither pH measurement nor impedance measurement was performed (4 patients, 66%), and weight regaining (2 patients, 33.3%).
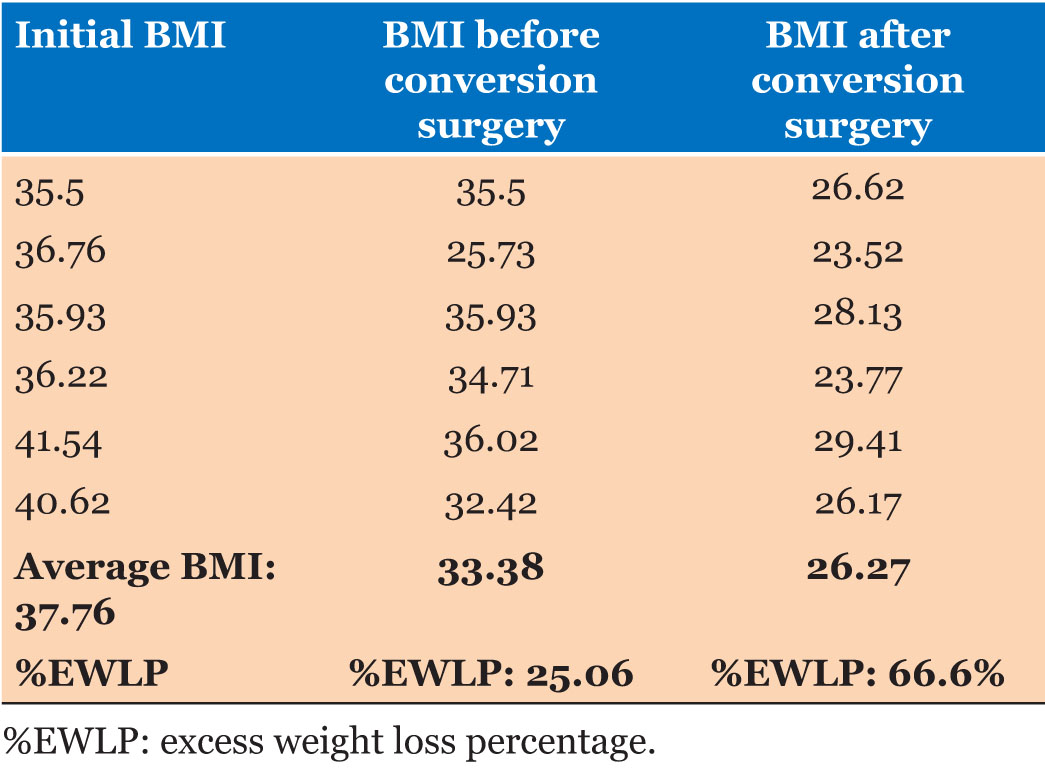
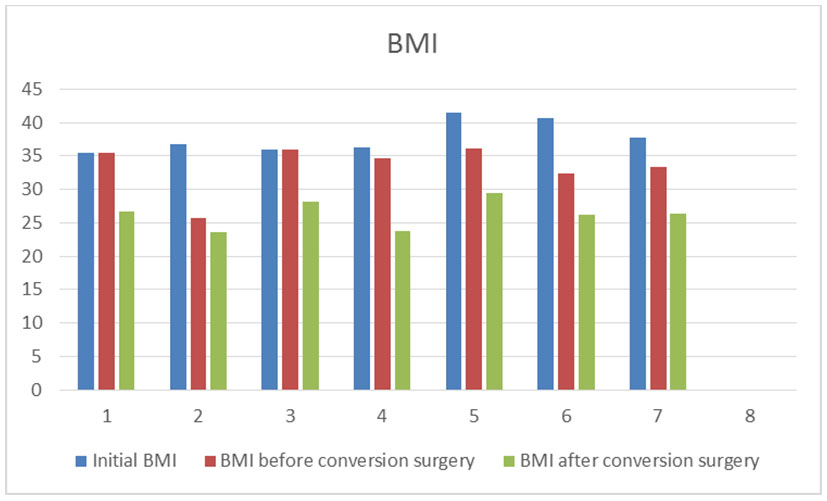
Before conversion surgery, the average weight was 91 kg with BMI of 33.38 kg/m2, and with excess weight loss percentage (%EWLP) of 25.06%. Indeed, not all had the same monitoring time after the first surgery. The time elapsed from the first surgery to conversion surgery was 58.3 months. In all surgeries the intraoperative findings were residual stomach dilation. Only one surgery presented a hiatal hernia in which plication of the diaphragmatic pillars was performed. However, after conversion surgery, there was a control in 7.1 months (averaged time). The average weight was 71.5 kg which corresponds to a 26.27 kg/m2 BMI and a %EWLP of 66.6% (Table 2) (Figure 1).
The same survey allowed to ask the patients about their satisfaction grade after surgery, in relation to weight loss, reflux symptoms, and eliminating or reducing clinical treatment. It was assessed from 1 to 10, where 1 was the least score (not satisfactory) and 10 was the maximum score (completely satisfactory). The results were highly favorable, with answers that indicated a 10 score in 5 patients and 9 in the one remaining patient. Correspondingly, patients who experienced GRD before conversion surgery, currently do not present symptoms.
DISCUSSION
The percentage of conversion surgeries at Police Hospital in Quito is 18.5%. This hospital is not a reference center for bariatric surgery. However, it has begun to perform obesity-related surgeries with a few patients.
In contrast, it has to be considered that one-half (9.25%) of the patients were from the institution, as their first surgery was performed at this health center, while the other half underwent surgery at different health centers. It is similar to the study published by Noah J. Switzer, Shahzeer Karmali (2016), who reported that 5–10% of the laparoscopic sleeve surgeries require conversion surgery [10]. Similarly, Aguilar (2020) mentioned that 5% and 11% of the laparoscopic sleeve surgeries will require a conversion surgery [3].
The average age of the patients surgically treated in this health center was 48 years, 66% were women and 33.3% were men. Results are in agreement with Abrham Abdemur’s report which stated that in 2015, average age of the patients was 46.5 years with 64.4% women and 35.5% men [6].
Weight loss after conversion surgery was notorious. Before the procedure, average weight was 91 kg whereas after the conversion surgery it was 71 kg. Consequently, BMI decrease 7 points with a final average of 26.27 kg/m2. These results are in agreement with Abraham Abdemur’s report, with an average BMI after conversion surgery of 28.6 kg/m2 (Figure 1) [6].
In this study, weight loss after first surgery of LSG was poor, as %EWLP was 25.06%. Nevertheless, the %EWLP was 66.6% after conversion surgery in 7.1 months monitoring. Similar reports showed a %EWLP of 65.5% after conversion as the one presented by Antonio Ianelli, with 15.6 months monitoring in 2016 [11].
Gastroesophageal reflux disease resolution was observed in all patients of the present study. Then, it has been demonstrated to be an effective treatment, in accordance with the results obtained by Tigran Poghosyan in his work published in 2016 [7]. Whereas Chetan (2017) suspended medication due to the absence of symptoms of GRD in 80% of the patients [12].
Satisfaction level and posterior life quality of the patients are factors that prevail in our study, because patients lost weight, the reflux symptoms were controlled and most of them stopped utilizing their usual medication. Therefore, their acceptance with regard to the surgical procedure was considered by purposing to rate it from 1 to 10 according to their satisfaction level. Here, a positive average of 9.83/10 was obtained whereby it was demonstrated that this surgical practice significantly improves patients’ life standards.
CONCLUSION
Conversion surgery is frequent, as laparoscopic sleeve gastric surgery is the most frequent bariatric procedure performed in the world. Conversion surgical intervention from LSG to RYGB warranties patients a reduction in reflux symptoms.
The weight loss percentage noticeably improves after conversion surgery from LSG to RYGB. Furthermore, it reduces co-morbidities related to obesity.
Patient’s satisfaction level is a variable that some studies have not given the importance that it deserves, therefore, our health center has decided to frequently measure this aspect to be able to demonstrate the improvement in patients’ life quality.
REFERENCES
1.
2.
Landreneau JP, Strong AT, Rodriguez JH, et al. Conversion of sleeve gastrectomy to Roux-en-Y gastric bypass. Obes Surg 2018;28(12):3843–50. [CrossRef]
[Pubmed]

3.
Aguilar-Espinosa F, Montoya-RamÃrez J, Gutiérrez Salinas J, Blas-Azotla R, Aguilar-Soto OA, Becerra-Gutiérrez LP. Conversion to Roux-en-Y gastric bypass surgery through a robotic-assisted hybrid technique after failed sleeve gastrectomy: Short-term results. [Article in Spanish]. Rev Gastroenterol Mex 2020;85(2):160–72. [CrossRef]
[Pubmed]

4.
Boru CE, Greco F, Giustacchini P, Raffaelli M, Silecchia G. Short-term outcomes of sleeve gastrectomy conversion to R-Y gastric bypass: Multi-center retrospective study. Langenbecks Arch Surg 2018;403(4):473–9. [CrossRef]
[Pubmed]

5.
Malinka T, Zerkowski J, Katharina I, Borbèly YM, Nett P, Kröll D. Three-year outcomes of revisional laparoscopic gastric bypass after failed laparoscopic sleeve gastrectomy: A case-matched analysis. Obes Surg 2017;27(9):2324–30. [CrossRef]
[Pubmed]

6.
Abdemur A, Han SM, Lo Menzo E, Szomstein S, Rosenthal R. Reasons and outcomes of conversion of laparoscopic sleeve gastrectomy to Roux-en-Y gastric bypass for nonresponders. Surg Obes Relat Dis 2016;12(1):113–8. [CrossRef]
[Pubmed]

7.
Poghosyan T, Lazzati A, Moszkowicz D, et al. Conversion of sleeve gastrectomy to Roux-en-Y gastric bypass: An audit of 34 patients. Surg Obes Relat Dis 2016;12(9):1646–51. [CrossRef]
[Pubmed]

8.
Quezada N, Hernández J, Pérez G, Gabrielli M, Raddatz A, Crovari F. Laparoscopic sleeve gastrectomy conversion to Roux-en-Y gastric bypass: Experience in 50 patients after 1 to 3 years of follow-up. Surg Obes Relat Dis 2016;12(8):1611–5. [CrossRef]
[Pubmed]

9.
Raj PP, Bhattacharya S, Misra S, et al. Gastroesophageal reflux-related physiologic changes after sleeve gastrectomy and Roux-en-Y gastric bypass: Acprospective comparative study. Surg Obes Relat Dis 2019;15(8):1261–9. [CrossRef]
[Pubmed]

10.
Switzer NJ, Karmali S, Gill RS, Sherman V. Revisional bariatric surgery. Surg Clin North Am 2016;96(4):827–42. [CrossRef]
[Pubmed]

11.
Iannelli A, Debs T, Martini F, Benichou B, Ben Amor I, Gugenheim J. Laparoscopic conversion of sleeve gastrectomy to Roux-en-Y gastric bypass: Indications and preliminary results. Surg Obes Relat Dis 2016;12(8):1533–8. [CrossRef]
[Pubmed]

12.
Parmar CD, Mahawar KK, Boyle M, Schroeder N, Balupuri S, Small PK. Conversion of sleeve gastrectomy to Roux-en-Y gastric bypass is effective for gastro-oesophageal reflux disease but not for further weight loss. Obes Surg 2017;27(7):1651–8. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Jhony A Delgado - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Juan P Torres - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Víctor H Paredes - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Alberto C Gordillo - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Gabriela J Racines - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Paola A Palacios - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2020 Jhony A Delgado et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.