|
Case Report
Superior mesenteric artery syndrome: Which treatment to be undertaken
1 MD, Resident in Visceral Surgery Department II, Mohammed V Training Military Hospital, Mohammed V University, Faculty of Medicine and Pharmacy, Rabat, Morocco
2 Professor, Visceral Surgery Department II, Mohammed V Training Military Hospital, Mohammed V University, Faculty of Medicine and Pharmacy, Rabat, Morocco
3 Professor, Chief of Visceral Surgery Department II, Mohammed V Training Military Hospital, Mohammed V University, Faculty of Medicine and Pharmacy, Rabat, Morocco
Address correspondence to:
Prosper Nsengiyumva
MD, Resident in Visceral Surgery Department II, Mohammed V Training Military Hospital, Mohammed V University, Faculty of Medicine and Pharmacy, Postal Code: 10045, Rabat,
Morocco
Message to Corresponding Author
Article ID: 100050S05PN2020
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Nsengiyumva P, Anajjar M, Fadili A, Elhjouji A, Ehrichiou A, Ait Ali A. Superior mesenteric artery syndrome: Which treatment to be undertaken. Edorium J Surg 2020;7:100050S05PN2020.ABSTRACT
Introduction: Superior mesenteric artery syndrome is an extrinsic compression of the third duodenal portion by the clamp formed by the aorta and the superior mesenteric artery consequentially to the loss of perivascular fatty tissue.
Case Report: We report a case of an old lady followed for Helicobacter pylori gastritis who was admitted in emergency room for postprandial vomiting, abdominal pain with hemodynamic instability and skin folds of dehydration. Biological assessment revealed severe hydroelectrolytic disorders, very low fat balance. Computer tomography (CT) scan requested discovered a significant reduction in space and aorto-mesenteric angle. After medical treatment during three days, the patient has undergone laparotomic gastro-entero-anastomosis with best immediate postoperative evolution. The late postoperative was marked by gastroparesis and cardiovascular complication.
Conclusion: The superior mesenteric syndrome is a rare entity. Abdominal CT scan is sufficient for diagnosis and no consensus was reached with regard to its management.
Keywords: Aorta, Duodenal extrinsic compression, Gastro-entero-anastomosis, Superior mesenteric artery
INTRODUCTION
Also known as Wilkie syndrome is a duodenal obstruction resulting from compression of the third duodenal portion during the passage between superior mesenteric artery and the aorta, following the disappearance of perivascular fatty tissue [1]. Thus, major burns, major surguries, cancer patients, malnourished patients, surgery involving traction on the mesentery, spinal deformity correction surgery are the risk factors of predisposition to this syndrome [2],[3]. Clinical findings of duodenal obstruction are epigastric pain, vomiting, anorexia, and weight loss [1]. Surgical treatment is recommended in case of failure of medical treatment [1]. Our concern is what the best treatment is and when to undertake it.
CASE REPORT
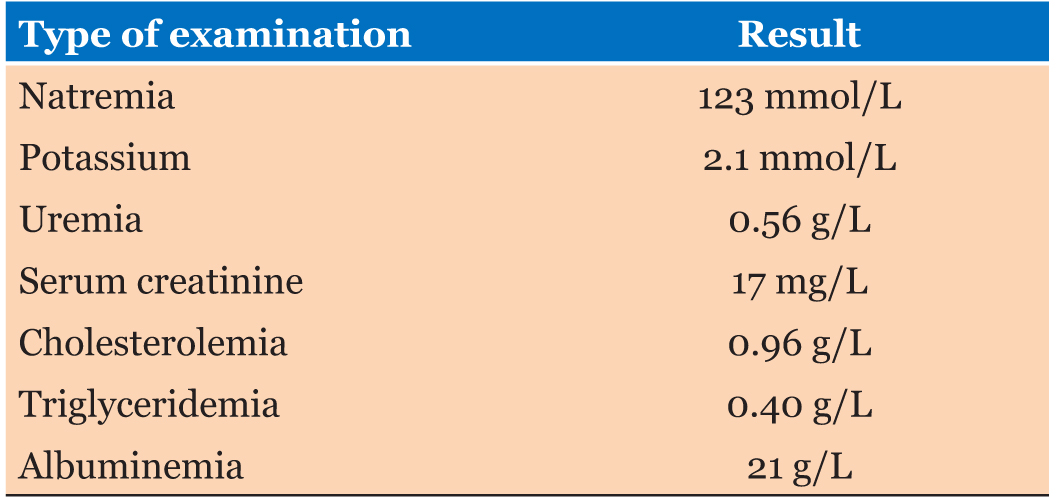
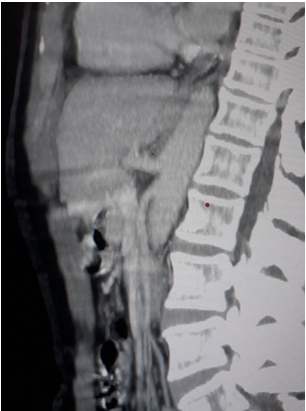
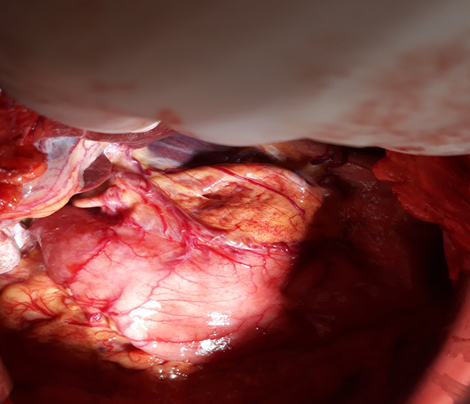
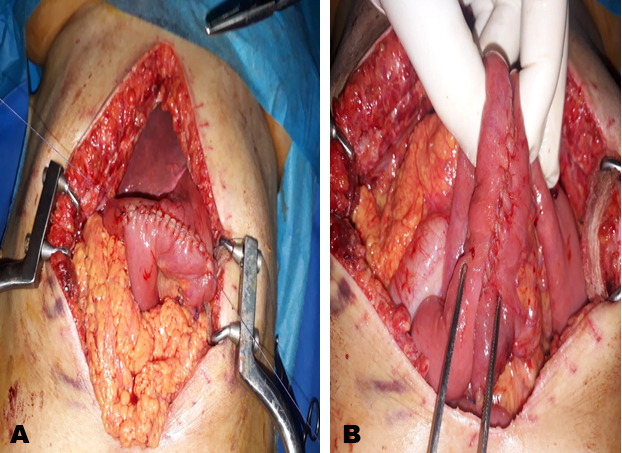
A 64-year-old female patient widowed followed for Helicobacter pylori gastritis who was admitted in emergency room for anorexia, vomiting, abdominal pain, and weight loss evolving context of deterioration in general condition since three months. Clinical examination revealed a hypotension with blood pressure of 80/40 mmHg, heartbeat of 130 beat per minute, body mass index (BMI) of 15.08 kg/m2, skin folds of dehydration, and epigastric region lapping. The biological assessment was disturbed as recorded in Table 1. An abdominal computed tomography (CT) scan requested urgently demonstrated a reduction in the aorto-mesenteric space not exceeding 5 mm with aorto-mesenteric angle measuring 19° (Figure 1). Medical management was first undertaken: urinary catheter, nasogastric tube, parenteral fluid, and electrolyte supplies within 72 hours without therapeutic success. Thus, a surgical option was undertaken with a laparotomic approach: supra-umbilical midline incision. On exploration, we found a duodenal and gastric distension upstream of the obstacle while the small intestine was collapsed downstream of the obstacle (Figure 2). The surgical procedure performed was gastro-entero-anastomosis (Figure 3A and Figure 3B), the nasogastric tube was removed two days after the surgery and oral feeding was authorized five days postoperative. The good clinical and biological evolution allowed the patient to be discharged ten days postoperative.
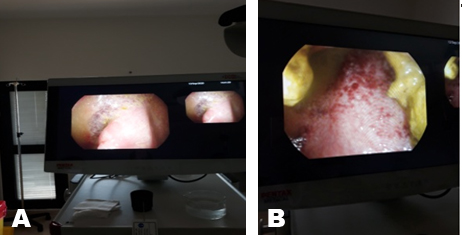
However, five days after discharging, the patient was readmitted to hospital for intermittent vomiting. Then, both biological and radiological investigations led to the conclusion of the diagnosis of gastroparesis (delay gastric emptying). The following arguments led to confirm this diagnosis: persistence of hydroelectrolytic disorders; disruption of the glycemic cycle; anastomotic permeability evidence on frontal abdominal X-ray performed after ingestion of product of contrast (poc) showing gastric atony and the presence of product in the small intestine (Figure 4). Thus, medical treatment based on prokinetics was instituted. The patient presented melena which led to perform a colonoscopy coupled with biopsies which highlighted at 15 cm from the anal margin an erythematous area and ulcerations mucosa at 30 cm from the anal margin (Figure 5A and Figure 5B). The histological examination of the biopsies concluded to subacute ulcerative rectosigmoiditis of non-specific appearance with foci of high-grade dysplasia, subacute mucoerosive colitis with foci of low-grade dysplasia, and other foci of high-grade.
Following the patient’s hemodynamic instability, she was transferred to the intensive care unit where she died.
DISCUSSION
In 1927, Wilkie described the first series of 75 patients and since then this syndrome bears his name [1]. While the duodenum is protected by fatty tissue perivascular, this syndrome occurs during rapid weight loss following the decompensation of a pre-existing tare [2],[4]. Our patient had clinical manifestations: vomiting, abdominal pain, while other studies reported a chronic clinical expression made up of repeated postprandial plenitudes and intermittent vomiting [1],[2]. In our patient, the angle between the superior mesenteric artery and the aorta was 19° and the aorto-mesenteric space was reduced to 5 mm while the normal values of the angle and the aorto-mesenteric space are respectively 25° and 60 at 10 mm and 28 mm [1],[5]. The goal of treatment is to break the dehydration and malnutrition caused by duodenal occlusion [4]. The effectiveness of medical treatment is estimated at 72% while recurrence is about 30% of cases [6]. However, the duration of medical treatment varies between two and twelve days even if a period of 169 days of successful treatment has been reported in child case study [1],[6]. For our patient, given her precarious nutritional state, BMI collapsed, a period of three days was granted for medical treatment. Several surgical techniques have been described, either derivation by gastro-jejunostomy or duodeno-jejunostomy or mobilization and uncrossing of the duodeno-jejunal angle by positioning the jejunum to the right of the superior mesenteric artery after sectioning the Treitz ligament according to Strong [1]. However, Strong’s procedure is not practicable in all patients due to duodenal distension with failure risk [1]. Our patient underwent a gastro-entero-anastomosis dictated by local conditions: duodenal and gastric distension.
Concerning her gastroparesis, a diet low in fat and fiber was recommended [7]. Prokinetics associated with the correction of the blood sugar, which was disturbed in our patient, by using insulin therapy allowed our patient to progress positively [8],[9].
CONCLUSION
Superior mesenteric artery syndrome is rare, sometimes unrecognized entity. Delay in diagnosis and treatment can cause dramatic consequences. The abdominal CT scan is a simple and powerful examination to make the diagnosis. Surgical treatment is only recommended in case of failure of medical treatment and a major challenge persists in the management of this syndrome. In addition, several complications can be associated with this syndrome.
REFERENCES
1.
Welsch T, Büchler MW, Kienle P. Recalling superior mesenteric artery syndrome. Dig Surg 2007;24(3):149–56. [CrossRef]
[Pubmed]

2.
Roy A, Gisel JJ, Roy V, Bouras EP. Superior mesenteric artery (Wilkie’s) syndrome as a result of cardiac cachexia. J Gen Intern Med 2005;20(10):C3–4.
[Pubmed]

3.
Zadegan F, Lenoir T, Drain O, Dauzac C, Leroux R, Morel E, Guigui P. Superior mesenteric artery syndrome following correction of spinal deformity: Case report and review of the literature. [Article in French]. Rev Chir Orthop Reparatrice Appar Mot 2007;93(2):181–5. [CrossRef]
[Pubmed]

4.
Bauer S, Karplus R, Belsky V, Mha HA. Superior mesenteric artery syndrome: A forgotten entity. Isr Med Assoc J 2013;15(4):189–91.
[Pubmed]

5.
Unal B, Akta? A, Kemal G, et al. Superior mesenteric artery syndrome: CT and ultrasonography findings. Diagn Interv Radiol 2005;11(2):90–5.
[Pubmed]

6.
Shin MS, Kim JY. Optimal duration of medical treatment in superior mesenteric artery syndrome in children. J Korean Med Sci 2013;28(8):1220–5. [CrossRef]
[Pubmed]

7.
Pilichiewicz AN, Horowitz M, Holtmann GJ, Talley NJ, Feinle-Bisset C. Relationship between symptoms and dietary patterns in patients with functional dyspepsia. Clin Gastroenterol Hepatol 2009;7(3):317–22. [CrossRef]
[Pubmed]

8.
Schvarcz E, Palmér M, Aman J, Horowitz M, Stridsberg M, Berne C. Physiological hyperglycemia slows gastric emptying in normal subjects and patients with insulin-dependent diabetes mellitus. Gastroenterology 1997;113(1):60–6. [CrossRef]
[Pubmed]

9.
Petrakis IE, Vrachassotakis N, Sciacca V, Vassilakis SI, Chalkiadakis G. Hyperglycaemia attenuates erythromycin-induced acceleration of solid-phase gastric emptying in idiopathic and diabetic gastroparesis. Scand J Gastroenterol 1999;34(4):396–403. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Prosper Nsengiyumva - Drafting the article, Final approval of the version to be published
Mohammed Anajjar - Acquisition of data, Revising it critically for important intellectual content, Final approval of the version to be published
Aziz Fadili - Analysis of data, Revising it critically for important intellectual content, Final approval of the version to be published
Abderrahman Elhjouji - Analysis of data, Revising it critically for important intellectual content, Final approval of the version to be published
Abdelkader Ehrichiou - Revising it critically for important intellectual content, Final approval of the version to be published
Abdelmounaim Ait Ali - Substantial contributions to conception and design, Revising it critically for important intellectual content, Final approval of the version to be published
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2020 Prosper Nsengiyumva et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.