|
Research Article
Wound preparation with locally adapted negative pressure dressing method: A comparative prospective study
1 Division of Plastic Surgery, Alex Ekwueme Federal University Teaching Hospital Abakaliki, Ebonyi State, Nigeria
2 Department of Surgery, Nnamdi Azikiwe University Teaching Nnewi, Anambra State, Nigeria
3 Plastic Surgery Division, Department of Orthopaedics, University of Benin Teaching Hospital Benin City, Edo State, Nigeria
4 Department of Obstetrics and Gynaecology, Alex Ekwueme Federal University Teaching Hospital Abakaliki, Ebonyi State, Nigeria
Address correspondence to:
Charles Chidiebele Maduba
PMB 102 Abakaliki, Ebonyi State,
Nigeria
Message to Corresponding Author
Article ID: 100051S05CM2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Maduba CC, Nnadozie UU, Modekwe VI, Ozoba FC, Anikwe CC, Nwankwo EU. Wound preparation with locally adapted negative pressure dressing method: A comparative prospective study. Edorium J Surg 2021;8:100051S05CM2021.ABSTRACT
Aims: The burden of chronic leg ulcers in resource poor settings outweighs the hospital capacity. This could be minimized with negative pressure dressing. We compared the rate of wound bed preparation using conventional and locally adapted negative pressure dressing methods.
Methods: Ninety-one patients enrolled in the study were assigned to either group managed respectively with locally adapted negative pressure and conventional dressing methods. Wound bed readiness was assessed clinically and microbiologically. The data collected with a proforma and were analyzed with IBM SPSS version 21. P-values less than 0.05 were statistically significant.
Results: There were 46 and 45 patients in groups A and B, respectively. The wound beds were ready in an average period of 11.6±7.40 days for group A and 28.8±16.67 days for group B which was statistically significant.
Conclusion: The locally adapted negative pressure wound dressing is a useful alternative to customized devices in ensuring rapid wound bed readiness.
Keywords: Conventional dressing, Customized vacuumassisted closure, Locally adapted negative pressure dressing, Wound bed preparation
INTRODUCTION
Management of chronic wounds could be very challenging to the surgeon and resource demanding to the patient [1]. Chronic wounds are wounds that fail to progress through normal phases of healing and so do not heal within 4–6 weeks of supervised conservative management or were unable to show 20–40% reduction following two to four weeks of supervised conservative management [2]. These wounds which arise mainly from poorly managed injuries in developing countries and vascular insufficiency in developed countries fail to progress through the normal phases of wound healing [1],[3]. They have economic, social, physical, and psychological impacts on the patients. Despite the advancement in wound care there is still much of the wounds that would not heal conservatively and so require surgical procedures to heal [1]. Lower extremity ulcers in the United States affect about 2.4–4.5 million people. It occurs in younger age group in developing countries [4]. This has an enormous economic impact in the productive work force and economy of the nation [5]. This therefore creates a necessity to hasten the healing process and minimize economic losses. Not only are there economic losses, the hospital facility is overwhelmingly stretched by the burden of in-patient care [6]. These could be reduced by adequate wound bed preparation that could reduce length of hospital stay.
Wound bed preparation requires tissue management, infection control, moisture balance, and edge/epithelial advancement (commonly known as TIME principle) [7]. This is done to promote conditions that enhance wound healing. Usually chronic wounds are stuck in one of the phases of wound healing which requires wound bed preparation to progress in the healing process [7]. The use of negative pressure wound therapy has been found to contribute significantly in wound bed preparation [8]. It works by creating a vacuum effect on the wound bed which stimulates granulation tissue formation, drains exudates and bio-burden, reduces wound edema, maintains moisture balance, and creates mechanical and biological creep effect on the wound edge leading to its advancement [9]. Apart from tissue management, other components of the TIME principle and much more are achieved by this. They have been shown to improve wound bed readiness with an average duration of about 14 days before they are ready for split-thickness skin grafting [8].
The negative pressure wound therapy devices also known as vacuum-assisted closure (VAC) devices have been produced in various customized forms. These are however very costly and hardly affordable to patients in the low and middle income countries (LMIC) who need them more [10]. It is therefore necessary to devise a locally adapted negative pressure wound therapy device which would be affordable and achieve the same effects as the customized types.
The aim of this study is to compare the duration of wound bed preparation of leg ulcers prior to surgical resurfacing with split-thickness skin grafting using conventional and locally adapted negative pressure dressing methods respectively.
MATERIALS AND METHODS
This is a prospective comparative study carried out in a tertiary hospital in Southeast Nigeria. Patients were recruited for the study from the surgical clinics and through consults from other surgical and medical specialties. The inclusion criteria included all wounds that fail to heal by conservative management, recurrent wounds; longstanding first time wounds that fail to heal prior to presentation, and wounds that would result to cosmetically unacceptable and unstable scars if allowed to heal by secondary intention. Those excluded in the study were patients who had poorly controlled systemic diseases like diabetes mellitus, HIV/AIDS, organ system failure and hemoglobinopathis, as well as patients on chemotherapy, smokers, and those on prolonged systemic steroids. Malignant ulcers, arterial ulcers, and wound beds with underlying chronic osteomyelitis were also excluded from the study.
Ethical approval was obtained from the research and ethics committee of Alex Ekwueme Federal University Teaching Hospital Abakaliki. A total of 91 patients who gave consent for the study were enrolled. They were assigned by convenient sampling method in which patients are added in alternate succession to either of the two groups A and B. Group A had locally adapted negative wound dressing while group B had conventional wound dressing. There were 46 patients in group A and 45 in group B. Prior to the commencement of each method of wound bed preparation, the wound was debrided.
The group A patients had locally adapted negative pressure dressing which was set up using a suction machine connected to a size 20 Fr feeding tube to the wound bed. The tube was additionally fenestrated and passed through a polyurethrane foam which was applied on the gauze layer placed on the wound bed. An airtight seal was achieved over the foam dressing using an Opsite or other transparent occlusive dressing materials (Figure 1). The suction negative pressure of 125 mmHg was maintained for 16 hours per day at 2 hours on and 1 hour off regimen. The dressings were changed every three days till the wound was considered adequate for surgical wound cover.
The group B patients had wound bed preparation using the conventional dressing with 5% povidone iodine mixed with equal volume of honey. Medical grade Laser honey was used in all cases to ensure uniformity. Dressings were changed on alternate day basis till the wound bed was considered adequate. The assessment of wound bed adequacy was clinical finding suggestive of healthy granulation tissue and laboratory finding of negative culture of wound swab using Levine method. Clinical wound bed adequacy was made by a blinded assessor. All patients who had clinical and/or laboratory evidence of wound infection were placed on antibiotics till the infections were eradicated. Empirical therapy was used in the first 48–72 hours till the culture and sensitivity results were available. Targeted therapy was then switched to with change in drugs where necessary. Local dressing antiseptics were maintained throughout the period of wound bed preparation.
Clinical photographs were taken at inception and following change of dressings to monitor progress of both conventional method (Figure 2 and Figure 3) and negative pressure dressing method (Figure 4 and Figure 5). Data on demographics, Hematocrit, serum albumin, ulcer size, ulcer duration, and duration of wound bed preparation were collected using a study proforma. Data was keyed into and analyzed using IBM SPSS statistics spreadsheet for windows (version 21.0; IBM Corp., Armonk, New York). Categorical data were analyzed for count and comparison done with Pearson Chi-square. Continuous variables were analyzed for mean and standard deviation, and comparison done with Mann–Whitney U test. P-values less than 0.05 were considered statistically significant.
Results
There were a total enrollee of ninety-one (91) for the study, 46 in group A and 45 in group B.
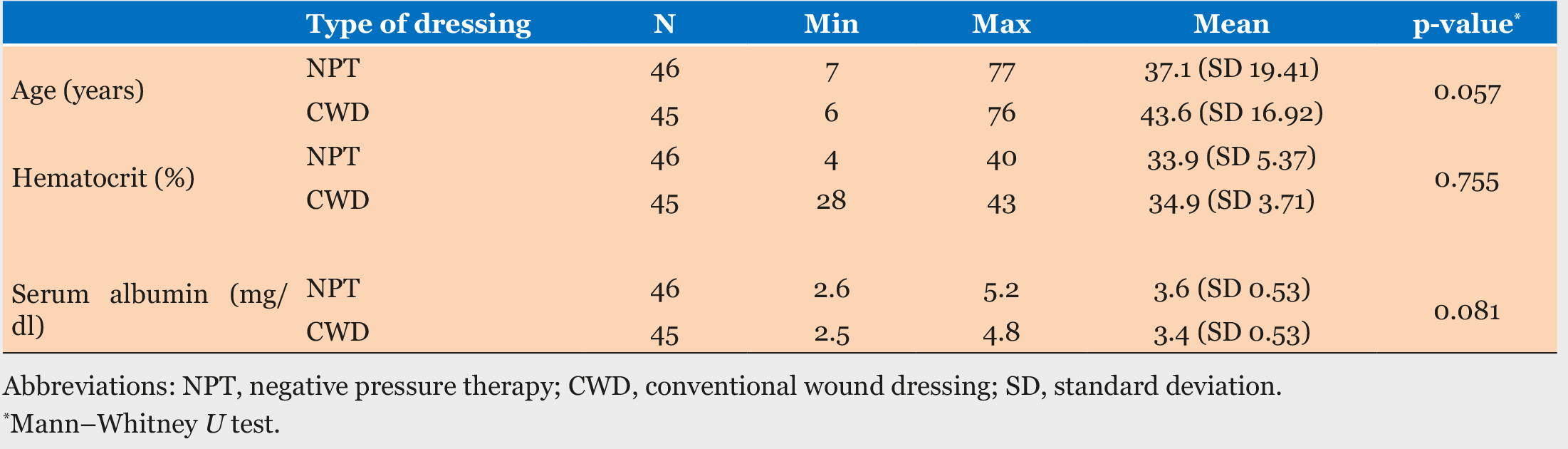
The patients aged between 6 and 77 years were enrolled for the study (Table 1). The group A patients had an average hematocrit of 33.9±5.55% while that of the group B patients was 34.9±3.71%. There was no statistical difference in the mean hematocrit of the two groups, with a p-value of 0.897. There was also no statistical difference between the mean serum albumin levels of the two groups at a p-value of 0.085 (Table 1).
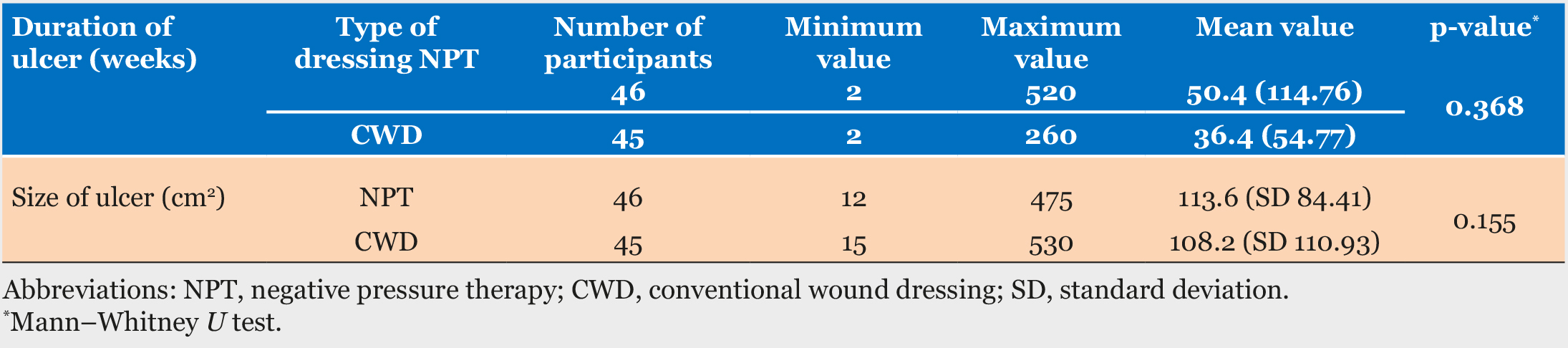
The mean duration of ulcers prior to commencement of dressing were 50.4 (SD 114.76) days and 36.4 (SD 54.77) days for groups A and B, respectively. There was no statistical difference between their mean values (p-value of 0.368) (Table 2). The mean sizes of the wounds for the two groups were 113.6 (SD 84.41) and, 108.2 (SD 110.93) respectively. This was not statistically significant with a p-value of 0.155 (Table 2).
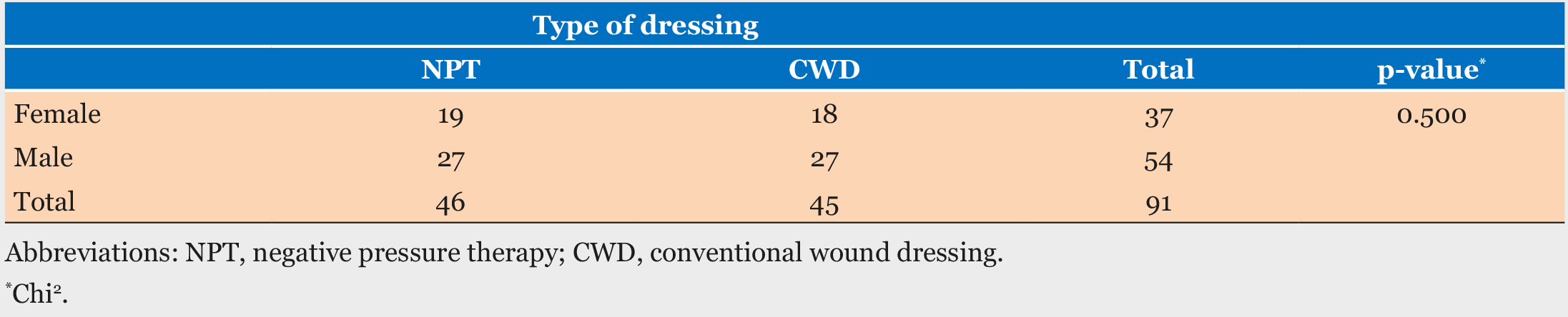
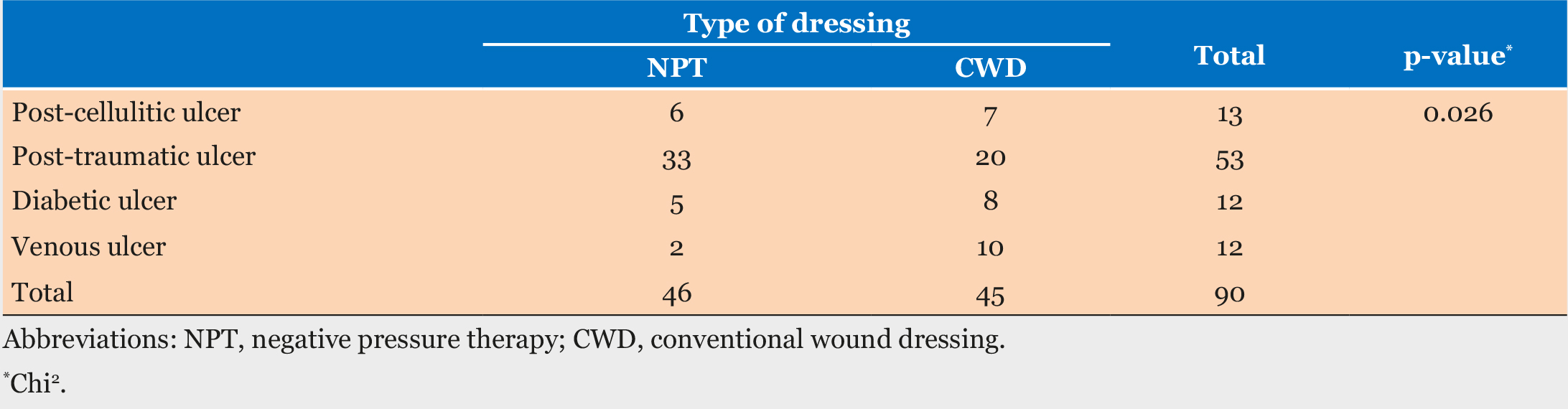
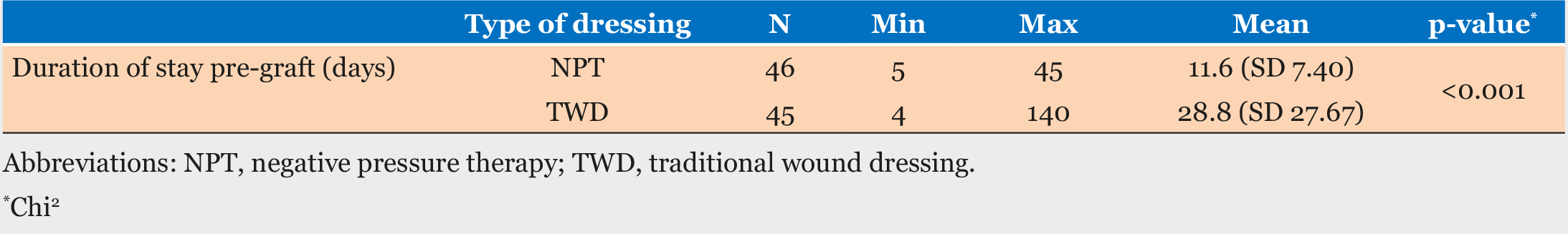
There were 54 males and 37 females with a male to female ratio of about 1.5:1 (Table 3). The leading cause of wound was trauma. Post-cellulitic ulcers were just marginally higher than both diabetic and venous ulcers which contributed in 12 cases each (Table 4). The majority of the wound affected the distal third of the leg while the proximal third had the least. The duration of dressing however was statistically significant between the two dressing methods. The negative pressure dressing method had an average duration of 11.6(+7.40) days while the conventional dressing method had an average wound bed preparation period of 28.8(+27.67) days. This was statistically significant with a p-value was less than 0.001 (Table 5).
DISCUSSION
The use of negative pressure wound therapy to prepare wound beds for ultimate surgical cover like split-thickness skin grafting and flap cover has been known as an important option in improving the surgical outcome [11]. This has been achieved with use of customized negative wound pressure therapy devices which are relatively unaffordable to most patients in resource limited settings [8]. Many adaptations are being tried to achieve the same results while mitigating the financial burden of this method of treatment [12],[13],[14].
A very crucial goal of wound bed preparation is to reduce the length of hospital stay. This could be achieved when the time required in preparing the wound before definitive treatment is significantly reduced. In a study using the customized negative pressure dressing to prepare wound beds, a significant success was made in reducing the duration of wound preparation [8].
In this study, we discovered an average wound bed preparation period of 11.6(+7.40) days using negative pressure dressing. This was statistically significant with a p-value less than 0.001 when compared with the conventional wound dressing method which had an average period of 28.8(+27.67) days. The possible conflicting factors such as the level of serum albumin, gender, hematocrit, and the effect of ageing on wound healing were all statistically insignificant [15]. Wound healing is impaired by poor nutrition in form of both protein-energy malnutrition and elemental/vitamin deficiencies. Serum albumin is a parameter for assessing protein nutritional status in surgical patients. Protein is one of the most essential macronutrients necessary for wound healing especially for granulation tissue formation in form of collagen and others [15]. Anemia on the other hand impairs wound healing as it reduces distribution of both oxygen and nutrients to the tissues. Wound healing is also known to be slower in the elderly due to reduced inflammatory and immune response [15]. These factors probably did not affect the rate of wound bed readiness for surgical cover in both groups.
The difference in the duration of wound bed preparation would ultimately contribute to the duration of the overall length of hospital stay. The reduction in the duration of wound bed preparation would not only reduce the cost of care on the patient or the funding organization but would also reduce the burden on the hospital facility.
Modifications are being employed with the aim of reducing cost and relieving the inpatient burden on the healthcare facilities [9]. The apparatus used in this study is one of the modifications capable of achieving the desired goal at a minimal cost. By achieving a wound bed preparation time which is was approximately 40% of the required time for preparation using conventional dressing, the length of stay and the cost of treatment would have significantly reduced.
In a resource poor setting, there are limited health facilities for managing recalcitrant ulcers. Hence, there is a need to ensure a rapid wound management protocol that could readily avail bed spaces for other waiting patients. There is also a need to ensure availability of options that are affordable to the patients. The suction machine being readily available in most hospitals in the developing countries provides a useful adaption for negative wound therapy. The other components, the feeding tube, the foam and the Opsite, are also relatively available. We therefore recommend a routine use of the negative pressure wound dressing in these setting to achieve the goal of reducing both the cost of care and the duration of stay in the hospital. This could be used in all categories of health facilities in developing countries since the apparatus is basically simple and easy to set up.
The major limitation of this study is that it is a single center study and would require multicenter studies to strengthen our conclusion. However, a similar study in another center in the same region showed a reduced hospital stay in patients who had split-thickness skin grafts dressed with similar modification of negative pressure dressing but at a lower vacuum pressure [16]. Secondly, we did not analyze the financial implication of the two forms of dressing. However at the time of this study there was no additional financial requirement for using the suction machine. Patients were only required to procure the feeding tube and foam. The hospital provided the Opsite and other similar airtight dressing materials at a subsidized price for all routine uses.
CONCLUSION
Locally adapted negative pressure wound dressing is a reliable alternative to the customized vacuum assisted closure device in wound bed preparation. It is capable of achieving wound bed readiness at such a rapid rate commensurate to the customized type, reducing the length of time spent in the hospital preparatory to definite surgical cover when the conventional wound dressing is employed. It is therefore recommended for use in wound bed preparation to ensure reduced length of stay and pressure on the limited health care facilities in the resource poor settings.
REFERENCES
1.
Frykberg RG, Banks J. Challenges in treatment of chronic wounds. Adv Wound Care (New Rochelle) 2015;4(9):560–82. [CrossRef]
[Pubmed]

2.
3.
4.
Rahman GA, Adigun IA, Fadeyi A. Epidemiology, etiology, and treatment of chronic leg ulcer: Experience with sixty patients. Ann Afr Med 2010;9(1):1–4. [CrossRef]
[Pubmed]

5.
Assadian O, Oswald JS, Leisten R, Hinz P, Daeschlein G, Kramer A. Management of leg and pressure ulcer in hospitalized patients: Direct costs are lower than expected. GMS Krankenhhyg Interdiszip. 2011;6(1):Doc07. [CrossRef]
[Pubmed]

6.
Lindholm C, Searie R. Wound management for the 21st century: Combining effectiveness and efficiency. Int Wound J 2016;13 Suppl 2:5–15. [CrossRef]
[Pubmed]

7.
8.
Jiburum BC, Opara KO, Nwagbara IC. Experience with vacuum-assisted closure device in the management of benign chronic leg ulcers. J West Afr Coll Surg 2011;1(1):89–100.
[Pubmed]

9.
Hussain A, Singh K, Singh M. Cost effectiveness of vacuum-assisted closure and its modifications: A review. International Scholarly Research Notices 2013;2013(595789):5. [CrossRef]

10.
Chiummariello S, Del Torto G, Iera M, Arleo S, Alfano C. Negative pressure dressing in split-thickness skin grafts: Experience with an alternative method. Wounds 2013;25(11):324–7.
[Pubmed]

11.
Fernández L. The utility of negative pressure wound therapy with instillation for wound bed preparation. Chronic Wound Care Management and Research 2019;2019(6):51–8. [CrossRef]

12.
Maduba CC, Nnadozie UU, Modekwe VI, Onah II. Split skin graft take in leg ulcers: Conventional dressing versus locally adapted negative pressure dressing. J Surg Res 2020;251:296–302. [CrossRef]
[Pubmed]

13.
Nguyen TQ, Franczyk M, Lee JC, Greives MR, O’Connor A, Gottlieb LJ. Prospective randomized controlled trial comparing two methods of securing skin grafts using negative pressure wound therapy: Vacuum-assisted closure and gauze suction. J Burn Care Res 2015;36(2):324–8. [CrossRef]
[Pubmed]

14.
15.
Guo S, DiPietro LA. Factors affecting wound healing. J Dent Res.2010;89(3):219–29. [CrossRef]
[Pubmed]

16.
Maduba CC, Nnadozie UU, Modekwe VI, Nwankwo EU. Comparing hospital stay and patient satisfaction in a resource poor setting using conventional and locally adapted negative pressure wound dressing methods in management of leg ulcers with split skin grafts: A comparative prospective study. Pan Afr Med J 2020;36:105. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Acknowledgments
We acknowledge the efforts of senior residents and plastic nurses who assisted in the research voluntarily.
Author ContributionsCharles Chidiebele Maduba - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Ugochukwu Uzodimma Nnadozie - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Victor Ifeanyichukwu Modekw - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Fidelis Chinedum Ozoba - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Chidebe Christian Anikwe - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Ezekiel Uchechukwu Nwankwo - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Charles Chidiebele Maduba et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.