|
Case Report
Cholecystocholedochal fistula and choledocolithiasis of great elements: A surgical challenge
1 MD, General surgeon, Division of General Surgery/Laparoscopy, Centro Médico de Especialidades, Hospital General de Ciudad Juárez, Ciudad Juárez, Chihuahua, Mexico
2 MD, General surgeon, Division of General Surgery/Laparoscopy, Centro Médico de Especialidades, Ciudad Juárez, Chihuahua, Mexico
3 MD, General physician, Instituto de Ciencias Biomédicas, Universidad Autónoma de Ciudad Juárez, Ciudad Juárez, Chihuahu, Mexico
4 MD, General physician, Escuela de Medicina y Ciencias de la Salud, Universidad Autónoma de Guadalajara, Zapopan, Jalisco, México
Address correspondence to:
Danai Hernández Carreón
Vicente Guerrero 8907, Fraccionamiento Las Quintas, CP 32401, Ciudad Juárez, Chihuahua,
Mexico
Message to Corresponding Author
Article ID: 100061S05CJ2025
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Jaime CAL, Aviléz CTP, Cereceres SJR, Carreón DH, De La Garza ASP. Cholecystocholedochal fistula and choledocolithiasis of great elements: A surgical challenge. Edorium J Surg 2025;11(1):1–6.ABSTRACT
Introduction: Choledocholithiasis, the most frequent complication of cholelithiasis, is defined as the presence of stones in the common bile duct. Mirizzi syndrome, a rare complication of cholelithiasis, appears with the impaction of stones in Hartmann’s pouch. Large element choledocholithiasis is considered when stones measure ≥15 mm.
Case Report: A 36-year-old female patient arrived at the emergency department presenting acute abdominal pain in the epigastrium, irradiated to the right hypochondrium accompanied by vomiting, choluria, and acholia. Hepatobiliary ultrasound showed cholelithiasis plus dilation of the bile ducts. Preoperative tests showed hyperbilirubinemia of 7.46 mg/dL with an obstructive pattern and alteration of liver function tests. Endoscopic retrograde cholangiopancreatography was performed and failed to mobilize the stone. During surgery a scleroatrophic gallbladder was identified without being able to identify the cystic duct and artery, suspecting a cholecystocholedochal fistula. A choledochotomy of 30 mm was performed to begin laparoscopic bile duct exploration. The extraction of 3 stones was achieved, the largest measuring 29 mm in diameter. Afterward, partial cholecystectomy was performed and a T-tube was placed through the choledochotomy. Intraoperative cholangiography was performed through a T-tube with adequate passage into the extrahepatic bile ducts toward the duodenum. Currently the patient is in her late postoperative period with a satisfactory evolution.
Conclusion: Secondary choledocholithiasis is a common disease as a complication of chronic cholelithiasis that, thanks to multiple advances, has been easily resolved due to ERCP with sphincterotomy and balloon sweep. However, there are cases such as choledocholithiasis of large elements in which its resolution through ERCP is not feasible.
Keywords: Choledocholithiasis, Cholelithiasis, Jaundice, Mirizzi syndrome
INTRODUCTION
Choledocholithiasis is defined as the presence of stones or calculi in the common bile duct and is classified as primary and secondary depending on its origin. Primary choledocholithiasis occurs when the stones form directly within the bile ducts and are composed mainly of calcium bilirubinate; these stones are rare in Western countries and more common in Asia. There are well-established criteria to define primary choledocholithiasis, which involve previous cholecystectomy without bile duct exploration, detection of choledocholithiasis at least two years after cholecystectomy and no evidence of biliary stricture prior to surgery. Nevertheless, most cases of choledocholithiasis are secondary, caused by the migration of gallstones, formed mainly by cholesterol, from the gallbladder into the common bile duct by gallbladder contractions [1],[2],[3].
Choledocholithiasis is the most frequent complication of cholelithiasis and represents about 18% of the complications, while Mirizzi syndrome is an unusual complication which occurs in approximately 0.1% of patients with gallstones. Choledocholithiasis incidence increases with age, approximately 25% of symptomatic patients have stones in the gallbladder, as well as in the common bile duct. Choledocholithiasis may present in different sizes. It is considered a large element choledocholithiasis when the stones measure ≥15 mm, while stones measuring ≥50 mm are gigantic. Up to 50% of choledocholithiasis cases may be asymptomatic [1],[4],[5],[6].
Mirizzi syndrome, a rare complication of cholelithiasis, appears with the impaction of stones in the cystic duct or in the Hartmann’s pouch. Continuous impaction of gallstones may lead to attacks of acute cholecystitis [6].
CASE REPORT
A 36-year-old female patient with no significant medical history. The patient arrived at the emergency department presenting acute abdominal pain in the epigastrium irradiated to the right hypochondrium and ipsilateral shoulder after ingestion of fatty foods with an intensity of 10/10, exacerbating upon inspiration and without extenuating circumstances. The patient also presented nausea, vomiting, choluria, and acholia.
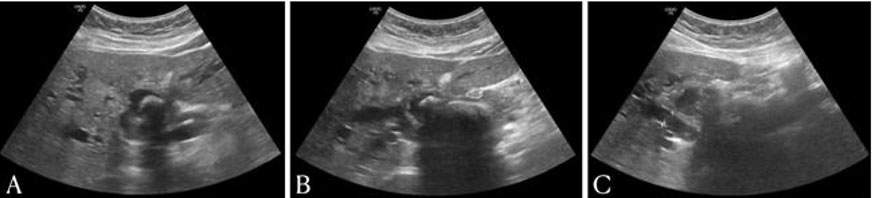
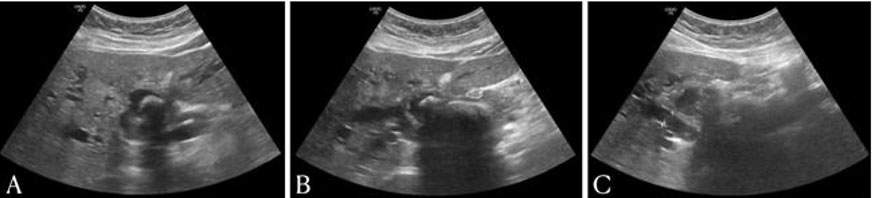
Physical examination reveals generalized jaundice, abdominal pain predominantly in the right upper quadrant on both superficial and deep palpation, with positive Murphy sign, and without evidence of peritoneal irritation. Diagnostic protocol was initiated based on hepatobiliary ultrasound demonstrating gallstones inside the gallbladder, wall thickness of 5 mm, dilation of the intrahepatic and extrahepatic bile ducts with a double-track sign, and the common bile duct diameter of 8.6 mm with probable calculi (Figure 1A, Figure 1B, Figure 1C). Preoperative tests showed neutrophilia, hemoglobin of 12.5 g/dL, platelets of 392,000, total bilirubin of 7.46 mg/dL with an obstructive pattern, direct bilirubin of 5.71 mg/dL, indirect bilirubin of 1.75 mg/dL, glutamic oxaloacetic transaminase of 186 U/L, glutamic pyruvic transaminase of 188.3 U/L, alkaline phosphatase of 458 U/L, gamma glutamyl transpeptidase of 581 U/L, total cholesterol of 233 mg/dL, and triglycerides of 208.7 mg/dL.
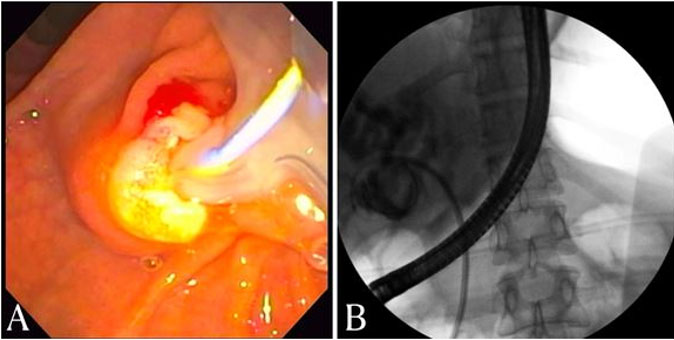
Due to the high probability of the patient having choledocholithiasis, an endoscopic retrograde cholangiopancreatography (ERCP) was performed. During the ERCP, dilation of the intrahepatic and extrahepatic bile ducts was observed with a common bile duct diameter of approximately 25 mm, and an oval filling defect in the proximal common bile duct with a diameter greater than 25 mm. A balloon was introduced, failing to mobilize the stone. Finally, a 10 cm × 10 cm French biliary stent was placed out (Figure 2A and Figure 2B). Post-ERCP diagnosis was unresolved large-element choledocholithiasis and to rule out Mirizzi syndrome.
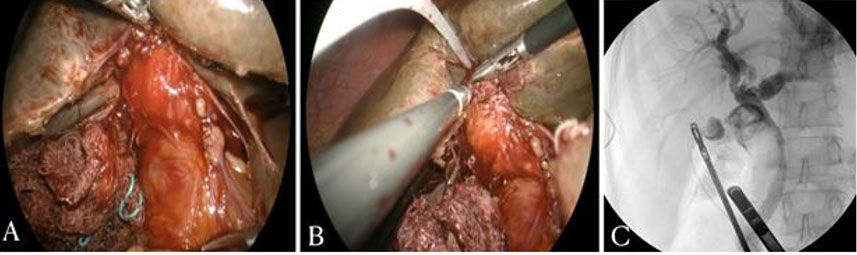
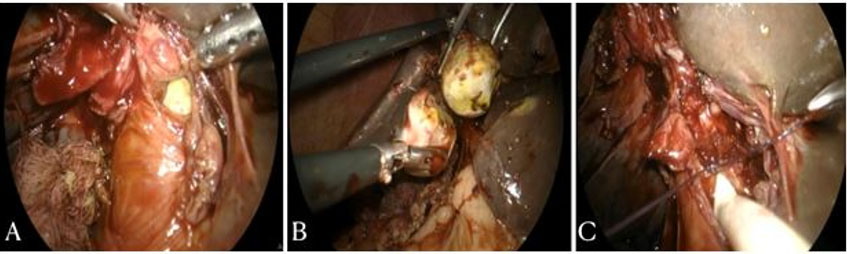
The patient was taken to the operating room, where, after general anesthesia and in a supine position, a laparoscopic cholecystectomy procedure was performed, identifying a large plastron in the right hypochondrium. Gallbladder fundus traction was performed, identifying a scleroatrophic gallbladder without being able to identify the cystic duct and cystic artery (Figure 3A). Therefore, a cholecystocholedochal fistula was suspected. Cholangiography through the gallbladder was performed in which contrast was observed at the gallbladder that passed at the level of the common bile duct through a large duct with evidence of large stones inside (Figure 3B and Figure 3C). Dissection of the gallbladder infundibulum toward the common bile duct and a choledochotomy of approximately 30 mm were performed to begin laparoscopic bile duct exploration (Figure 4A). The extraction of 3 stones was achieved, the largest measuring approximately 29 mm in diameter, and an endoprosthesis placed via ERCP was identified (Figure 4B and Figure 5). Afterward, partial cholecystectomy was performed with closure at the level of the infundibulum with 3-0 vicryl suture, continuous suture. Subsequently, a T-tube was placed through the choledochotomy, which was closed and fixed with a flap of the posterior wall of the gallbladder toward the choledochorrhaphy site (Figure 4C). Intraoperative cholangiography was performed through the T-tube with adequate passage into the intrahepatic and extrahepatic bile ducts toward the duodenum. The absence of leaks was verified and exhaustive surgical cleaning was carried out. The stones and gallbladder were placed in an endobag, which was extracted through the subxiphoid port. Hemostasis was verified and a drainage was placed on the right flank toward the surgical bed and the procedure was terminated. In the postoperative period, with satisfactory evolution, the penrose drainage was removed in the outpatient clinic one week after surgery. At the sixth week, a cholangiography via T-tube was performed without evidence of residual lithiasis and with adequate passage to the duodenum, which is why the T-tube was removed (Figure 6). Two weeks later, the patient underwent a new ERCP for endoprosthesis removal. Currently the patient is in her late postoperative period with a satisfactory evolution without complications.
DISCUSSION
Mirizzi syndrome is caused by an inflammatory process secondary to the erosion produced by an impacted gallstone and may result in partial or complete obstruction of the common bile duct. The inflammatory process favors the formation of adhesions, specially to the common bile duct, duodenum, and colon. The impacted gallstone in combination with the inflammatory process causes the external compression and obstruction, which will end up causing erosion of the mucosa and will progress to a cholecystohepatic, cholecystoduodenal, or cholecystocholedochal fistula. Mirizzi type 1 is the only one not involving a fistula. The presence of a cholecystocholedochal fistula increases the risk of bile duct injury during cholecystectomy. Preoperative diagnosis of Mirizzi syndrome is often difficult and more than 50% of patients are diagnosed during surgery. Intraoperative diagnosis is suggested by the presence of adhesions between the gallbladder and CBD, and by a contracted gallbladder. Within the classification of gallstones there is a definition for stones of difficult management with criteria such as diameter ≥15 mm, anatomical alterations of the common bile duct, impaction of the stone, or periampullary diverticulum. Multiple risk factors may contribute to choledocholithiasis including age, female gender, genetic predisposition, metabolic disorders, dietary habits, diabetic neuropathy, obesity, and rapid weight loss [6],[7],[8],[9],[10].
The appearance of clinical manifestations will depend on whether the stones produce partial or complete obstruction of the common bile duct. The main clinical manifestations are jaundice and right upper quadrant abdominal pain. Patients can also present acholia, choluria, fever, nausea, and vomiting. Laboratories may show leukocytosis, hyperbilirubinemia with an obstructive pattern, high alkaline phosphatase, and elevated transaminase levels [5],[6],[10],[11].
The initial suspicion of choledocholithiasis is based on symptoms, laboratory results, and ultrasound findings, which can all be used as a guide to establish the probability of choledocholithiasis. Endoscopic retrograde cholangiopancreatography (ERCP) is the diagnostic method and treatment of choice for patients with high probability of choledocholithiasis, while magnetic resonance cholangiopancreatography (MRCP) is reserved for cases of low or moderate probability [9],[12].
Transabdominal hepatobiliary ultrasound is the initial imaging study requested, which provides information on gallstones, in addition to CBD dilation. A diameter >6 mm is considered an indirect sign of choledocholithiasis. The confirmatory diagnosis is made with advanced imaging such as magnetic resonance cholangiopancreatography (MRCP), endoscopic retrograde cholangiopancreatography (ERCP), endoscopic ultrasound (EUS), intraoperative cholangiography (IOC), and percutaneous transhepatic cholangiography (PTC). The MRCP is considered the diagnostic method of choice for CBD stones. Endoscopic retrograde cholangiopancreatography is considered to be the best diagnostic method for Mirizzi syndrome and is capable of treating 90% of choledocholithiasis cases. It has the advantage of being a diagnostic and therapeutic procedure involving the cannulation of the ampulla of Vater and CBD with injection of contrast and observing for filling defects, which is used to evaluate the presence of stones in the CBD. Complications rates of the ERCP vary from 8–12%, the most common being pancreatitis [4],[10],[12].
The treatment of choledocholithiasis established by the American Society for Gastrointestinal Endoscopy (ASGE) and European Society for Gastrointestinal Endoscopy (ESGE) indicates endoscopic retrograde cholangiopancreatography as the first treatment option. Nowadays, ERCP is first performed using a sphincterotomy technique to extract the stones followed by laparoscopic cholecystectomy, which constitutes the two stage treatment most often chosen. Large element choledocholithiasis is a challenge for both the surgeon and the endoscopist. For stones smaller than 10 mm, ERCP is very effective; however, its effectiveness decreases as the stone size increases. Endoscopists with extensive experience in choledocholithiasis are usually able to extract stones larger than 10 mm, but it should be noted that the removal rate for stones larger than 15 mm using ERCP decreases to 12% even considering the endoscopist’s experience. Laparoscopic common bile duct exploration (LCBDE) is also recommended nowadays and has a complication rate similar to ERCP. The LCBDE can be divided in two categories: transcystic/transcholecystic and choledochotomy. The transcystic approach is appropriate for stones measuring less than 10 mm, while the choledochotomy is reserved for patients with dilation of the common bile duct greater than 10 mm and will allow retrieval of greater stones [8],[9],[11][12],[13].
The surgical treatment for Mirizzi syndrome widely differs depending on its classification. Laparoscopic subtotal cholecystectomy and laparoscopic cholecystectomy, fundus first approach, reduce the risk of biliary duct injury. Although laparoscopic cholecystectomy is not considered the standard treatment due to the difficulty involving adhesions and severe inflammation in Calot’s triangle with great risk of CBD injury, thus representing a great surgical challenge, with the right skills can be performed for Mirizzi syndrome type 1 and type 2. Endoscopic retrograde cholangiopancreatography may also be used as primary treatment or in conjunction with the surgical procedure. For cases involving a fistula, Mirizzi type 2 through 5, it is suggested to perform a cholecysto-choledocus-duodenostomy or can also be attempted the direct repair of the fistula by placing a T-tube [6],[10].
Choledocholithiasis may become complicated with cholangitis, biliary pancreatitis, and biliary perforation. In contrast, Mirizzi syndrome can become complicated with cholecystohepatic, cholecystoduodenal, or cholecystocholedochal fistula. However, the prognosis is Favorable when diagnosed and treated promptly. A coexistent carcinoma of the gallbladder with Mirizzi syndrome is possible due to the chronic and persistent inflammation. Gallbladder carcinoma, cholangiocarcinoma, pancreatic cancer, and sclerosing cholangitis should be included in the differential diagnosis [7],[10].
CONCLUSION
Secondary choledocholithiasis is a common disease as a complication of chronic cholelithiasis that, thanks to multiple advances, has been easily resolved due to ERCP with sphincterotomy and balloon sweep. However, there are cases such as choledocholithiasis of large elements in which its resolution through ERCP is not feasible. Therefore, it is suggested to perform cholecystectomy with exploration of the bile ducts, given that currently the ease of performing it laparoscopically is feasible. In this case, it was performed by removing large stones, as a consequence of chronic cholelithiasis with Mirizzi syndrome, which created a cholecystocholedochal fistula. The resolution of this case was laparoscopic with bile duct exploration, partial cholecystectomy, T-tube placement, and closure of the fistula with a flap of the posterior wall of the gallbladder. This is a highly complex case resolved by laparoscopic surgery that had a satisfactory evolution with low output through the T-tube.
Chronicity in patients with cholelithiasis in addition to episodes of exacerbation of cholecystitis leads to an even more complex surgical resolution, which is why in the presence of a patient with cholecystitis or cholelithiasis and an episode of exacerbation, early surgical resolution is suggested.
REFERENCES
1.
Lamichhane S, Kc S, Mishra N, Devkota S, Kumar A, Gupta RK. Giant primary choledocholithiasis: A rare case report and comprehensive review of literature. Clin Case Rep 2024;12(12):e9720. [CrossRef]
[Pubmed]

2.
Zhang J, Ling X. Risk factors and management of primary choledocholithiasis: A systematic review. ANZ J Surg 2021;91(4):530–6. [CrossRef]
[Pubmed]

3.
Cianci P, Restini E. Management of cholelithiasis with choledocholithiasis: Endoscopic and surgical approaches. World J Gastroenterol 2021;27(28):4536–54. [CrossRef]
[Pubmed]

4.
V V, S Kumar N, Khan O, Azharuddin SK. Giant choledocholithiasis with choledochal cyst: A report of a rare case. Cureus 2024;16(7):e64306. [CrossRef]
[Pubmed]

5.
6.
Shirah BH, Shirah HA, Albeladi KB. Mirizzi syndrome: Necessity for safe approach in dealing with diagnostic and treatment challenges. Ann Hepatobiliary Pancreat Surg 2017;21(3):122–30. [CrossRef]
[Pubmed]

7.
8.
9.
Akmal AM, Putra BP, Darmaningrat CIAA, Nariswari IGARC, Srigede LD, Budyono C. Management of cholelithiasis with concomitant choledocholithiasis. Acta Med Indones 2022;54(1):151–7.
[Pubmed]

10.
Valderrama-Treviño AI, Granados-Romero JJ, Espejel-Deloiza M, et al. Updates in Mirizzi syndrome. Hepatobiliary Surg Nutr 2017;6(3):170–8. [CrossRef]
[Pubmed]

11.
12.
Molvar C, Glaenzer B. Choledocholithiasis: Evaluation, treatment, and outcomes. Semin Intervent Radiol 2016;33(4):268–76. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Acknowledgments
We thank the staff of Centro Medico de Especialidades for their support and constant drive to learn.
Author ContributionsCesar Alberto López Jaime - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Carlos Tadeo Perzabal Aviléz - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Saul Jasam Ruiz Cereceres - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Danai Hernández Carreón - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Ana Sofía Perzabal De La Garza - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2025 Cesar Alberto López Jaime et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.